More Information
Submitted: December 28, 2020 | Approved: January 08, 2021 | Published: January 11, 2021
How to cite this article: Erkabu S, Taddese Z, Bearega B, Daniel E, Birhanu M. Acute urinary retention and hyponatremia from central hypothyroidism. J Neurosci Neurol Disord. 2021; 5: 001-003.
DOI: 10.29328/journal.jnnd.1001042
Copyright License: © 2021 Erkabu S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Acute urinary retention; Hyponatremia; Central hypothyroidism; Pituitary macro adenoma
Acute urinary retention and hyponatremia from central hypothyroidism
Samson Erkabu1*, Zerihun Taddese1, Biniam Bearega1, Eyuel Daniel1 and Mekonen Birhanu2
1Internal Medicine Department, Ras Desta Damtew Memorial Hospital, Addis Ababa, Ethiopia
2Department of Radiology, Saint Paul Millennium Medical College, Addis Ababa, Ethiopia
*Address for Correspondence: Samson Erkabu, MD, Internal Medicine Department, Ras Desta Damtew Memorial Hospital, Addis Ababa, Ethiopia, Tel: +251920762077; Email: [email protected]
A mass arising from the pituitary gland commonly damages cells of the anterior pituitary gland and affects the secretion of gonadotropins and growth hormone. However, central hypothyroidism and secondary adrenal insufficiency from such damage is a rare phenomenon. Acute urinary retention as the main symptom of central hypothyroidism is also an unusual initial presentation. We report a male patient who comes with frequent urinary retention and hyponatremia at our hospital.
Central hypothyroidism (CH) refers to thyroid hormone deficiency due to a disorder of the pituitary, hypothalamus, or hypothalamic-pituitary portal circulation. It is a rare cause of hypothyroidism, estimated to occur in 1:20,000 to 1:80,000 in the general population [1]. The causes of central hypothyroidism include pituitary or hypothalamic pathologies. The most frequent cause of central hypothyroidism is Pituitary macroadenomas [2]. The diagnosis of CH is suggested by the findings of low thyroid hormone concentrations, associated with inappropriately low/normal TSH levels. The clinical manifestations of Central Hypothyroidism are similar to those of primary hypothyroidism. Here we present a man who seeks medical attention for recurrent acute urinary retention and hyponatremia as a result of central hypothyroidism.
A 64- year old male hypertensive patient on nifedipine comes to the emergency room complaining of fatigue, persistent vomiting, loss of appetite, and epigastric discomfort accompanied by a failure to pass urine for a few days. He reported no headache, fever, seizure, or any form of abnormal body movement or body weakness. He had undergone supra-pubic prostatectomy years ago as he had bladder outlet obstruction secondary to benign prostatic hyperplasia.
At presentation, his vital signs were stable; his physical examinations were unremarkable except for lassitude. The blood workup showed a normal complete blood count and organ function tests. The serum electrolyte study was notable for hyponatremia.
The abdominal ultrasound revealed absent prostate otherwise normal findings. The hyponatremia was corrected, and the gastrointestinal symptoms were managed by anti-emetic and proton pump inhibitor. Since the patient had marked improvement symptomatically, he was discharged from the hospital.
After three weeks of discharge from the hospital, he comes again with a complaint of acute urine retention and difficulty walking. He also complained of easy fatigability, constipation, and change in mentation for few days. Upon physical examination; His vital signs were stable. The neurologic evaluation showed a confused man who was not oriented to place and time. His muscle strength and tone of all his extremities were decreased. The other findings were unremarkable.
A blood sample for complete blood count, renal function test, and blood glucose level were taken and reported normal. The serum electrolyte, however, revealed hyponatremia. This time thyroid function and other serum hormone study done, and the results are shown in tables 1 and 2.
| Table 1: Serum electrolytes. | ||||
| Serum electrolytes | ||||
| Date | ||||
| 04/07/2020 | 10/07/2020 | 14/07/2020 | 17/07/2020 | |
| Sodium | 122 mmol/L | 126 mmol/L | 128 mmol/L | 138 mmol/L |
| Potassium | 4.2 mmol/L | 3.7 mmol/L | 5.0 mmol/L | 3.6 mmol/L |
| Chloride | 91 mmol/L | 94mmol/l | 102 mmol/L | 103 mmol/L |
| Calcium | 8.8 mg/dl | 8.8 mg/dl | 9.4 mg/dl | 9.2 mg/dl |
| Table 2: Serum Hormonal levels. | |||
| Hormone studies | |||
|
|||
| Date | |||
| 09/07/20 | 13/08/20 | References | |
| TSH | 0.782 uU/ml | 1.410 uU/ml | 0.27-4.2 |
| Free T3 | 1.46 uU/ml | 1.65 uU/ml | 2.02-4.43 |
| Free T4 | 0.66 uU/ml | 1.07 uU/ml | 0.93-1.71 |
|
|||
| Date | References | ||
| 13/07/20 | |||
| Morning Serum ACTH | 2.94 pg/ml | 7.2-63.3 pg/ml | |
| Serum cortisol | 2.07 ug/dl | 6.2-19.4 ug/dl | |
| Prolactin | 4.36 ng/ml | 4-15.2 ng/ml | |
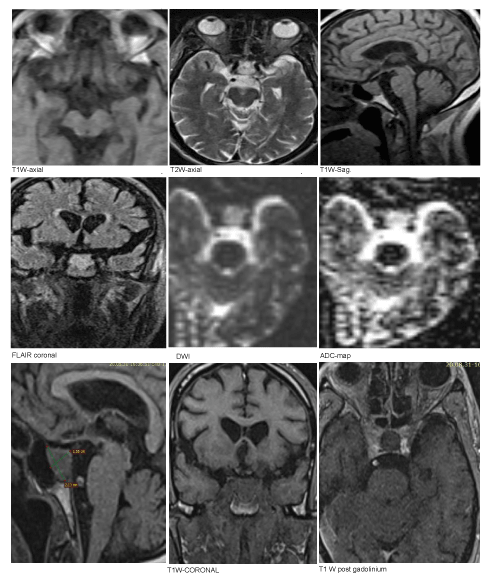
He was admitted to the general medical ward for further workup; with a working diagnosis of quadriparesis, hyponatremia, and acute urinary retention. Later the Magnetic Resonance Imaging (MRI) revealed a Pituitary macro-adenoma (Figure 1). The findings from Electromyogram (EMG) Test & Nerve Conduction Study (NCS) were suggestive of mild to moderate sensory-motor polyneuropathy.
Figure 1: MRI of the brain.
After the serum hormone studies, we started the patient on thyroxin 50 µg per day and prednisolone 7.5 mg per day. Within a few days of commencing the treatment, serum sodium level corrected, the confusion, fatigability, and constipation abated. After weeks of initiation of therapy the patient regained his full motor abilities and bladder function.
Hyponatremia is a common finding in a state of low thyroid hormones. However, acute bladder retention from peripheral neuropathies due to central hypothyroidism is an unusual initial clinical presentation. There are only a few case reports where bladder retention was a clinical presentation because of hypothyroidism. Urinary retention was found incidentally in a middle-aged woman who has all signs of hypothyroidism including myxedema, malaise a change in tone of voice [3]. There was also a report where a female patient had uremia from urinary retention and was found to have hypothyroidism [4]. In our case, we attribute the urinary retention of the patient to hypothyroidism related peripheral neuropathies as the patient responded well to thyroid hormonal replacement.
The most important mechanism of development of hyponatremia in a state of low thyroid hormone is the decreased capacity of free water excretion due to elevated antidiuretic hormone (ADH) levels [5,6].
In patients with myxedema, the accumulation of interstitial mucopolysaccharides results in fluid retention and decreased effective arterial blood volume leading to ADH-mediated water retention and reduced sodium levels [7,8].
Few hypothyroid patients have increased urine sodium concentration as a result of syndrome of Inappropriate ADH secretion and not to reduced cardiac output [9].
Secondary adrenal insufficiency is also related to hyponatremia through increased ADH secretion. In this particular patient, the low ACTH was suggestive of the presence of secondary adrenal insufficiency; and we believed some of the symptoms have abated by the introduction of prednisolone.
Urinary retention could be the presenting symptom of hypothyroidism, and frequent finding of hyponatremia from an unknown cause needs a warrant for thyroid hormone evaluation.
Ethical issues
Permission to report the case was given by the patient after discussing and consent was made.
- Persani L. Clinical review: Central hypothyroidism: pathogenic, diagnostic, and therapeutic challenges. J Clin Endocrinol Metab. 2012; 97: 3068. PubMed: https://pubmed.ncbi.nlm.nih.gov/22851492/
- Samuels MH, Ridgway EC. Central hypothyroidism. Endocrinol Metab Clin North Am. 1992; 21: 903–919. PubMed: https://pubmed.ncbi.nlm.nih.gov/1486881/
- Justo D, Schwartz N, Dvorkin E, Gringauz I, Groutz A. asymptomatic urinary retention in elderly women upon admission to the Internal Medicine department: A prospective study. Neurourol Urodyn. 2017; 36: 794-797. PubMed: https://pubmed.ncbi.nlm.nih.gov/27176656/
- Nathan AW, Havard CW. Paralytic ileus and urinary retention due to hypothyroidism. Br Med J (Clin Res Ed). 1982; 285: 477. PubMed: https://pubmed.ncbi.nlm.nih.gov/6809133/
- Derubertis FR, Jr, Michelis MF, Bloom ME, Mintz DH, Field JB, et al. Impaired water excretion in myxedema. Am J Med. 1971; 51: 41–53. PubMed: https://pubmed.ncbi.nlm.nih.gov/5570319/
- Hanna FW, Scanlon MF. Hyponatraemia, hypothyroidism, and role of arginine-vasopressin. Lancet. 1997; 350: 755–756. PubMed: https://pubmed.ncbi.nlm.nih.gov/9297992/
- Hierholzer K, Finke R. Myxedema. Kidney Int Suppl. 1997; 59: S82–S89. PubMed: https://pubmed.ncbi.nlm.nih.gov/9185111/
- Abuzaid AS, Birch N. The controversies of hyponatraemia in hypothyroidism: weighing the evidence. Sultan Qaboos Univ Med J. 2015; 15: e207–e212. PubMed: https://pubmed.ncbi.nlm.nih.gov/26052453/
- Archambeaud-Mouveroux F, Dejax C, Jadaud JM, Vincent D, Laroumagne G, et al. [Myxedema coma with hypervasopressinism. 2 cases]. Annales de Médecine Interne. 1987; 138: 114–118. PubMed: https://pubmed.ncbi.nlm.nih.gov/3579092/