More Information
Submitted: September 01, 2022 | Approved: September 09, 2022 | Published: September 10, 2022
How to cite this article: Dahshan I, Saad MM, Shora HA, Abbas H, Awad MM, et al. Knowledge, attitude and behaviour of undergraduate medical students towards mentally Ill patients-Suez Canal University, Egypt. J Neurosci Neurol Disord. 2022; 6: 034-039.
DOI: 10.29328/journal.jnnd.1001066
Copyright License: © 2022 Dahshan I, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Negative belief; Mental health; Medical students
Abbreviations: MAKS: Mental Health Knowledge Scale; BMI: Beliefs towards Mental Illness scale; RIBS: Reported and Intended Behavior Scale
Knowledge, attitude and behaviour of undergraduate medical students towards mentally Ill patients-Suez Canal University, Egypt
Ismail Dahshan1, Menna M Saad1, Hassan A Shora2* , Hanan Abbas1, Mohamed M Awad1, Omneya Y Ibrahim1 and Mohamed Abd El-Wahed1
, Hanan Abbas1, Mohamed M Awad1, Omneya Y Ibrahim1 and Mohamed Abd El-Wahed1
1Department of Family Medicine, Faculty of Medicine Suez Canal University, Ismailia, Egypt
2Senior Research Scientist, Head of Medicine & Diabetes Center, Port-Said University & Ismailia Medical Complex,, Egypt
*Address for Correspondence: Hassan A Shora, Senior Research Scientist, Head of Medicine & Diabetes Center, Port-Said University & Ismailia Medical Complex,, Egypt, Tel: +201224020233, Email: [email protected]
Background: Worldwide, studies show negative attitudes among medical students toward psychiatry and mental illness. The knowledge of the attitude and awareness of the undergraduate medical students toward mental health and psychiatric disorders are most important as they are going to be involved in the care of these patients either directly or indirectly during the years of their careers.
Aim: To explore, the knowledge, attitude, and behavior of undergraduate medical students towards mentally ill Patients before their planned psychiatry rotation in the fourth year of undergraduate medical study, faculty of medicine, Suez Canal University, Ismailia, Egypt.
Objectives: To assess mental health-related knowledge, attitudes and intended behavior of undergraduate medical students towards mentally ill patients.
Subjects and methods: A descriptive, cross-sectional study, conducted on 120 fourth-year undergraduate medical students affiliated with the faculty of medicine-Suez Canal University. A comprehensive sample was used to include all of the students in the fourth year of undergraduate medical study, and the study group participants completed a semi-structured questionnaire including four parts to assess their knowledge, attitudes, and behavioral responses towards individuals with mental illnesses. The data of the study was collected in September-October 2019.
Results: Based on the participants’ scores, the cut-off points estimated to dichotomize the responses as poor or good, for mental health-related knowledge, belief towards mental illness and intended behavior were, 17, 55 and 8.5 respectively. This study showed that the study participants had marginally poor mental health-related knowledge with a median score of 17, poor beliefs about mental illness with a median score of 49.5 and poor intended behavior towards the mentally ill with a median score of 7.
Conclusion: In this study, undergraduate medical students showed marginally poor mental health-related knowledge, poor stigmatizing beliefs, and behavior towards mentally ill patients. More controlled studies are needed to eliminate the inherent response biases in survey studies and to measure the outcomes of anti-stigma educational and curricular interventions.
Despite the wide prevalence of mental health problems in the general population, with an estimate of more than 1.1 billion people worldwide suffering from mental and substance use disorders, only 30% - 40% of mentally ill patients seek treatment [1,2]. People with mental illness die prematurely, WHO 2018 reported that 76% - 85% of people with mental disorders receive no treatment for their disorder in low and middle-income countries and 35% - 50% of people with mental disorders are in the same situation in high-income countries [2].
One of these reasons is that the physical healthcare provided is less appropriate than that provided to people without mental health problems [3]. There is a pressing need to improve these factors contributing to these inequalities. One of the reasons contributing to these disparities is stigmatization and discrimination against people with mental illness by healthcare professionals who share the general public’s stigmatizing views towards mentally ill patients [4]. Like the general public, medical students have also the stereotypical view that people with mental illness are unlikely to recover and can be dangerous [5].
Stigma and discrimination cause a significant burden for people suffering from psychiatric disorders. In the last years, many tools have been used to assess stigmatizing attitudes toward psychiatric patients [5,6]. Unfortunately, negative attitudes towards people with a psychiatric diagnosis are not confined to the lay public but are also common among health professionals [7,8]. So, it is important to assess medical students’ attitudes and behavior towards mentally ill patients, as they will be involved in the care of these patients throughout their careers in the future.
Subjects and sample size
The current study is a cross-sectional descriptive (survey) study, that was conducted in September 2019. It was carried out on 120 fourth-year undergraduate medical students, affiliated with the faculty of medicine, Suez Canal University in Ismailia city, Egypt, before joining their psychiatric rotation, to assess mental health-related knowledge, attitudes & intended behavior. A comprehensive sample was used to include all the students in the fourth grade. The sample size was calculated with a power of 80% and a level of significance of 0.05, based on a previously published study [9]. Permission for carrying out the study was obtained after completing all formalities and obtaining the ethical approval of the research and ethics committee of the faculty of medicine, at Suez Canal University. The participants and medical students were informed about the purpose of the study and signed informed consent before the beginning of this study.
The study participants were subjected to a semi-structured self-administrated questionnaire [10,11]. The questionnaire was designed to be used anonymously and reviewed by experts matter in the psychiatry department.
The questionnaire is composed of four parts
The first part: Consists of socio-demographic data of each medical student, which includes age, gender, family history of mental illness and contact with mentally ill patients in the past 3 months and if he/she received the previous year’s seminars or workshops related to the stigma of mental illness.
The second part: Consists of Specific items that measure mental health-related knowledge among the general public using the Mental Health Knowledge Schedule (MAKS), its validity is supported by extensive review by experts including service users and international experts in stigma research and has been found to be brief and feasible with internal reliability and test-retest reliability moderate to substantial [11]. Part A of the scale comprises six items covering stigma-related mental health knowledge areas (need for paid employment, advice for professional help, medication is effective, psychotherapy is effective, full recovery from mental illness, seeking professional help by mentally ill) and Part B consists of six items that inquire about the classification of various conditions as mental illnesses to help contextualize the responses to other items. A 5-point Likert scale was used, and response options range from 1 = totally disagree to 5 = totally agree. “Don’t know” was valued at 3 for the purposes of determining a total score. Items 6, 8 and 12 are reverse coded to reflect the direction of the correct response. The total score was calculated by adding the response values for only items 1–6 (Part A) and ranged from 6 to 30. A higher score indicates more knowledge. The Cronbach’s alpha for the MAKS scale was 0.749.
The third part: Used, the Beliefs towards Mental Illness scale (BMI) to assess the attitudes toward mental illness, the scale was designed to measure cross-cultural differences in such beliefs as well as to predict treatment-seeking behavior among different cultural groups, with reliability estimates for each factor revealed to be moderate to high internal consistency [12]. It is composed of 21 items that measure negative stereotypical views of mental illness.
The BMI scale consists of three subscales
Dangerousness subscale: Consists of five items (1, 2, 3, 6, 13) relating to the perceived dangerousness of mental illness and patients.
Social and interpersonal skills subscale: Consists of 10 items (4, 5, 8, 11, 12, 14, 15, 17, 18, 21) covering the effect of mental illness on interpersonal relationships and related feelings of despair. It assesses the level of frustration and despair in interpersonal relationships with individuals with a mental illness. Also, taps feelings of shame about mental illness and the perception that the mentally ill are untrustworthy.
Incurability subscale: Consists of six items (7, 9, 10, 16, 19, 20) covering perceptiveness of incurability of mental illness. Items are rated on a five-point Likert scale, reverse coded from 1 (strongly agreement) to 5(strongly disagree).
The total score was calculated by adding the response values for 21 items and ranged from 21 to 105. The lower score reflects a more negative belief toward the mentally ill. The Cronbach’s alpha for the BMI scale was 0.82 and the subscales were between 0.69 - 0.80.
The fourth part: Assesses the mental health-related reported and intended Behavior measured by the Reported and Intended Behavior Scale (RIBS), Which was found to be a brief, feasible and psychometrically robust measure for assessing health-related reported and intended behavioral discrimination, with moderate to substantial internal consistency and test-retest reliability [13]. The four reported behavior outcomes included, living with, working with, living nearby, and continuing a relationship with someone with a mental health problem, while the four-intended behavior outcomes assessed the future intended behavior of the same items. A 5-point Likert scale was used, and response options range from 1 = totally disagree to 5 = totally agree. “Don’t know” was valued at 3 for the purposes of determining a total score. The total score for each student is calculated by adding together the response values for intended behavior items and ranges from 4 to 20. A higher score indicates more favorable intended behavior. The Cronbach’s alpha for the RIBS scale was 0.75.
Ethical approval for carrying out the study was obtained from The Ethical Committee of the Faculty of Medicine, Suez Canal University, and the participant students were informed about the purpose of the study and signed informed consent before the start of the study.
Statistical analysis
The data of the current study were analyzed using the SPSS version 20 (i.e. statistical package for social sciences) program. According to the results of the Shapiro-Wilk test for normality, continuous data were expressed as the median and interquartile range (IQR). Spearman correlation coefficient test was conducted to find the correlation between medical students’ knowledge, attitude and behavior, toward mentally ill patients and different demographic variables. The scores of mental health-related knowledge, belief towards mental illness (with its 3 subscales), and intended behavior were categorized as poor or good based on the threshold score (cut-off point) obtained from the Likert scale which is ordinal but is often analyzed as numerical neglecting the differences between ordinal scores according to the following formula:
The threshold score = ([total highest score-total lowest score]/2) + total lowest score.
The results were presented as tables and graphs.
The mean age of students included in the study was 21.2 ± 0.4 and 53.3% of the participant students were females. 69.2% of the students were never in contact with people with mental illness in the past 3 months. 30% of the students had a family history of mental illness. No one of the study participants (0%) had received in the previous year, a seminar, workshop training or read an article about the stigma of mental illness (Table 1).
| Table 1: Socio-demographic characteristics of the undergraduate medical students (n = 120). | ||
| Variables | Frequency | % |
| Gender | ||
| Male | 56 | 46.7 |
| Female | 64 | 53.3 |
| Age (in years) (Median: IQR*) | 21 | 21:21 |
| Contact with people with mental illness in the past 3 months. | ||
| Never | 83 | 69.2 |
| Sometimes (once per month) | 29 | 24.2 |
| Often (once every 2 weeks) | 7 | 5.8 |
| Always (once per week) | 1 | 0.8 |
| Family history of mental illness. | 36 | 30.0 |
| Did you receive in the previous year any of the followings? | ||
| Seminar about the stigma of mental illness | 0 | 0.0 |
| Workshop training about the stigma of mental illness | 0 | 0.0 |
| Read an article about the stigma of mental illness | 0 | 0.0 |
| None | 120 | 100.0 |
| *IQR: interquartile range. | ||
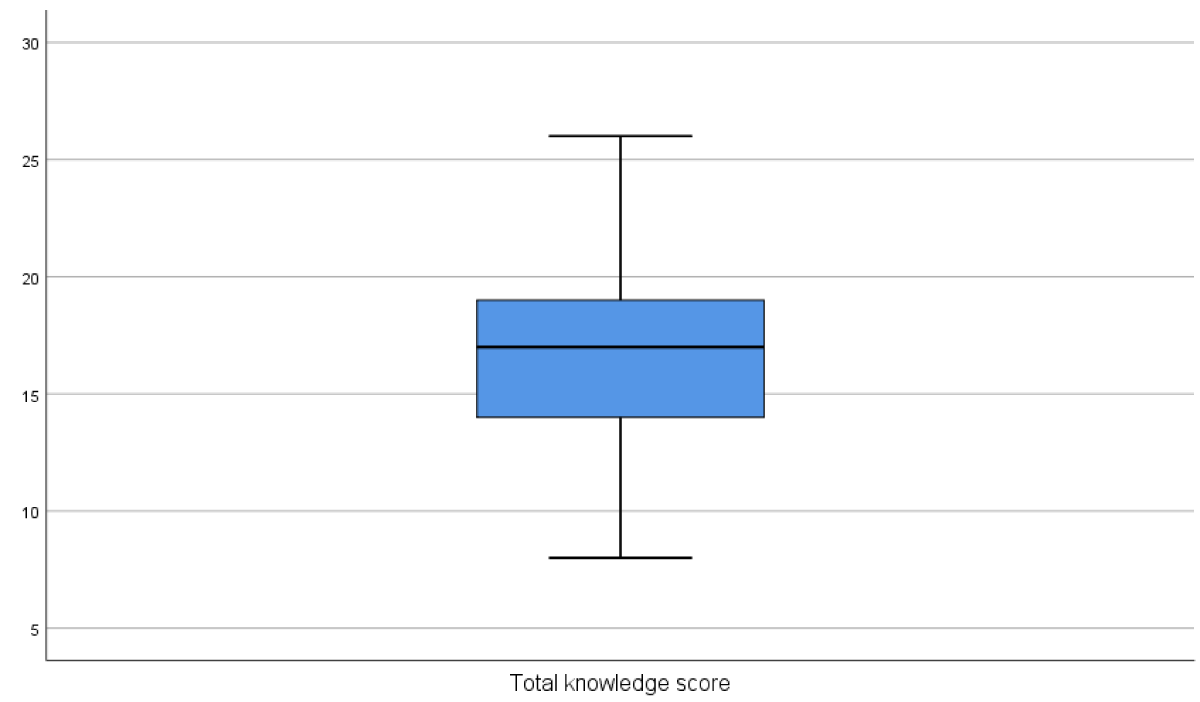
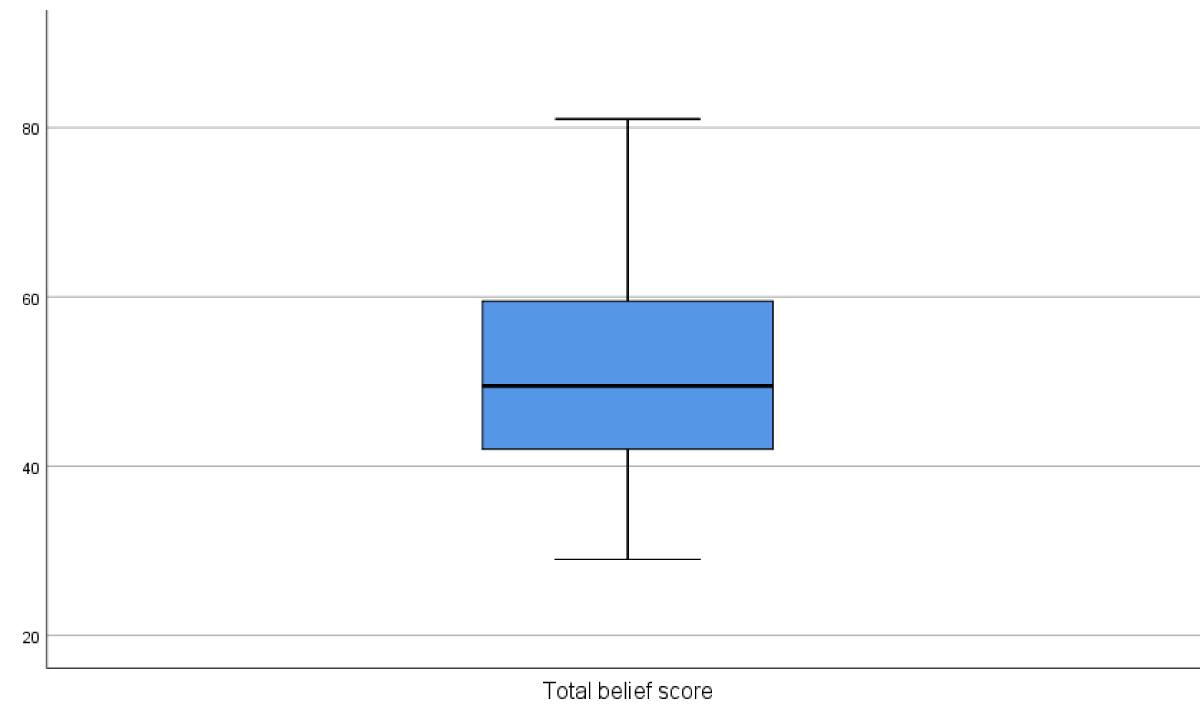
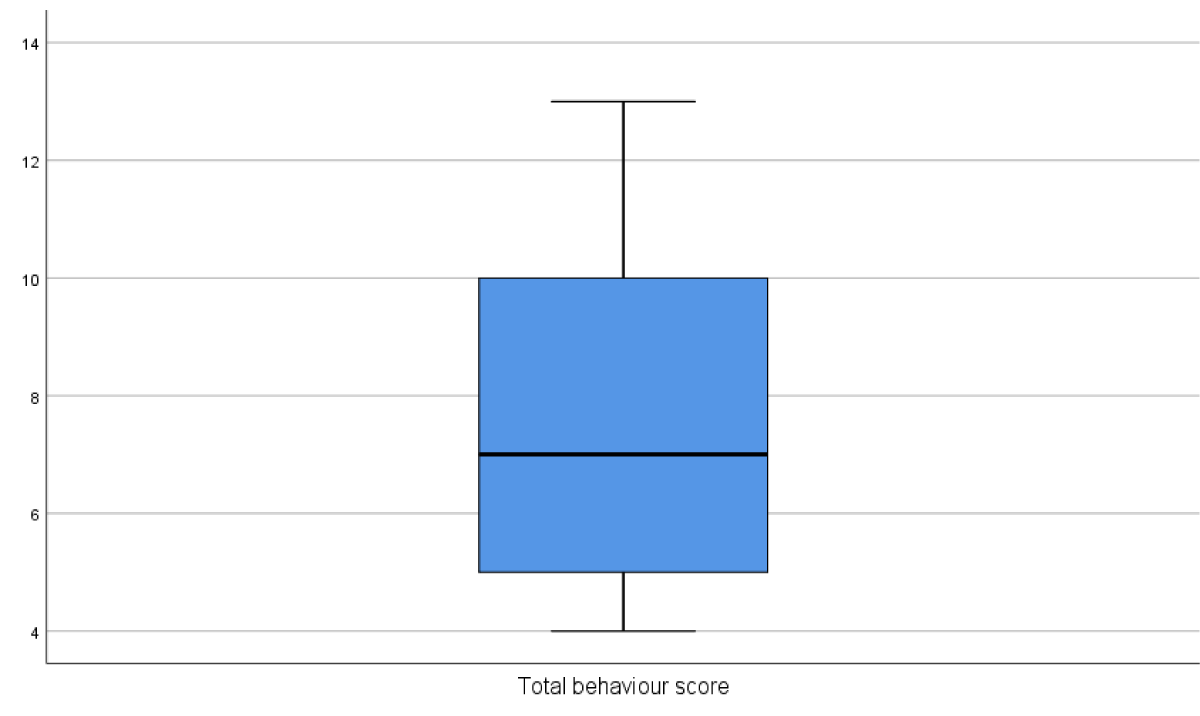
Based on the participants’ scores, the threshold scores (cut-off points) for mental health-related knowledge, belief towards mental illness and intended behavior were 17, 55 and 8.5 respectively. This study showed that the study participants had slightly poor mental health-related knowledge with a median score of 17, poor beliefs about mental illness with a median score of 49.5 and poor intended behavior towards the mentally ill with a median score of 7 (Table 2, Figures 1-3). The threshold scores (cut-off points) for the subscales of the Beliefs toward Mental illness scale (BMI) were 12.5, 27.5 and 15.5 for the dangerousness, social and interpersonal skills, and incurability subscales, respectively. Poor median scores were shown for the social and interpersonal skills, and incurability subscales 22 and 15, respectively, while a good median score of 14 was shown for the dangerousness subscales (Table 3).
Figure 1: Box Plot of mental health-related knowledge score of undergraduate medical students regarding mental illness.
Figure 2: Box Plot of beliefs towards mental illness score of undergraduate medical students.
Figure 3: Box Plot of intended behavior score of undergraduate medical students.
| Table 2: Median score with IQR* versus threshold levels of mental health-related knowledge, beliefs towards Mental Illness, and intended behavior scales of the undergraduate medical students (n = 120). | |||
| Variables | Median (IQR) | Threshold level (cut off Point) |
Range of the score |
| Mental health-related Knowledge | 17 (14 -19) | 17 | 6 - 30 |
| Belief in mental illness | 49.5 (42 - 59.5) | 55 | 21-105 |
| Intended behavior | 7(5 -10) | 8.5 | 4 - 20 |
| *IQR: interquartile range. | |||
| Table 3: Median scores with IQR* versus threshold levels of subscales of Beliefs towards Mental Illness scale of the undergraduate medical students (n = 120). | ||
| Subscales | Median (IQR*) | Threshold level (cut-off point) |
| Dangerousness | 14 (12 - 16) | 12.5 |
| Poor interpersonal and social skills | 22 (17 - 26) | 27.5 |
| Incurability | 15(12 - 17) | 8.5 |
| *IQR: interquartile range. | ||
Studying the relationship between sociodemographic data as predictors of change in beliefs and intended behavior towards mentally ill patients, contact with mentally ill patients in the last 3 months was a highly significant predictor of beliefs towards mental illnesses (p < 0.001), and family history of mental illness was also a significant predictor of future intended behavior (p < 0.025)(Table 4).
| Table 4: Linear regression of sociodemographic data as predictors of change in beliefs and intended behavior towards mental illness among undergraduate medical students (n = 120). | ||||||
| Unstandardized Coefficients | Standardized Coefficients | P value | 95.0% C.I for ß | |||
| ß | S.E. | Beta | Lower Bound | Upper Bound | ||
| (Constant) | 212.8 | 56.3 | < 0.001* | 101.2 | 324.3 | |
| Gender | 8.4 | 2.2 | 0.3 | < 0.001* | 4.1 | 12.7 |
| Age | 9.3 | 2.6 | 0.3 | < 0.001* | 4.2 | 14.5 |
| Contact with people with mental illness in the past 3 months as a predictor of change in beliefs towards mental illnesses. | 4.8 | 1.7 | 0.2 | < 0.001* | 1.4 | 8.1 |
| Family history of mental illness as a predictor of change in intended behavior towards mental illnesses. | 1.5 | 0.7 | 0.2 | 0.025* | 0.2 | 2.8 |
| *Statistically significant at p value < 0.05. | ||||||
There was a moderate correlation between the study participant students’ beliefs and their intended behavior toward mental illness scores (R = 0.47) (Table 5).
| Table 5: Spearman correlation between students’ knowledge, belief, and intended behavior of undergraduate medical students (n = 120). | |||
| knowledge score | belief score | intended behavior score | |
| knowledge score | - 0.01(0.881) | 0.03(0.753) | |
| belief score |
|
0.47(< 0.001*) | |
| Data presented as the correlation coefficient *Statistically significant at p value < 0.05. | |||
Stigma has been conceptualized as comprised of 3 constructs: knowledge (ignorance), attitudes (prejudice) and behavior (discrimination) [11]. The current study was carried out to describe mental health-related knowledge, attitude, and behavior of undergraduate 4th year medical students, Suez canal University, Egypt, towards mentally ill patients, using the Mental Health Knowledge Schedule (MAKS), Beliefs towards Mental Illness scale (BMI) that included, three different subscales (dangerousness, poor social and interpersonal skills, and incurability) and Reported and Intended Behavior Scale (RIBS), before their psychiatry rotation normally introduced in the fifth year of the undergraduate curriculum.
The results showed that the participant’s students had marginally poor mental health-related knowledge scores, poor stigmatized beliefs towards mental illness that was poor for interpersonal relationship and social skills and incurability subscales and good for dangerousness subscale, as well as a poor score of favorable intended behavior towards mental illness. In a study in Saudi Arabia by Shahrour & Rehmani to measure stigmatizing attitudes of the staff of King Abdul-Aziz Hospital toward mentally ill patients, the results showed, that discriminatory behavior against mentally ill patients could result from a feeling that these patients are dangerous), and that was explained by the possible influence of the culture of the medical community, which is historically had negative views of psychiatry and psychiatrists and by the negative role of media as radio, television, or newspaper and magazines, using stigmatizing words such as “mad” and “insane” [9]. Comparing the findings of our study with a similar descriptive study carried out by Chawla, et al, in India, undergraduate medical students were found to have multiple lacunae in their knowledge of psychiatry, psychiatric disorders, psychiatric patients and psychiatric treatment [14]. A Nigerian study done by James J, et al. on a sample of final years medical students and new graduates, showed that participants endorsed stigmatized attitudes towards the mentally ill, with an attitude more adverse for schizophrenia compared with depression [15]. another two studies done in India and Turkey, both examined the attitudes among medical students before and after exposure to psychiatric educational interventions, in the first study done by Poreddi V, et al. in India, there were generally negative attitudes toward mentally ill patients, that showed improvement in the benevolence, and stigmatization domains after the intervention [16], While, in the second study done in Turkey by Altindag A, et al. 2006, examining the effects of an anti-stigma program on medical students’ attitudes towards one of the most stigmatizing psychiatric disease (schizophrenia), favorable attitudinal changes was observed in terms of belief about the etiology of schizophrenia, social distance to people with schizophrenia and care and management of people with schizophrenia [17].
In this study, exploring the relationship between the socio-demographic data as predictors of change in different outcomes variables, there was a highly significant relationship between contact with mentally ill patients in the last 3 months, and beliefs (p < 0.001), and a significant relationship between family history of mental illness, and intended behavior (p = 0.025). Comparing these relationships with other studies, in a study done by Alaa El-Din MA, et al. 2016, in Egypt, who assess the impact of clinical psychiatric rotation at Ain- shams faculty of medicine on the attitude of undergraduate medical students, one of the study’s conclusions, showed that, medical students who had a positive family history of mental illness had a better attitude towards mental illness [18]. In another study in the UK by Hearn J & Marwood M who evaluated the medical students’ understanding of mental illness using the Mental Health Literacy Scale (MHLS) and their relationships with demographics and experiences with mental illness, concluded that having personal experience of mental illness, as well as having a close friend or family member with a mental illness was associated with higher MHL score [19].
A recent study carried out in Lebanon in 2019, used similar tools to assess knowledge, attitude and behavior, among the general public, and concluded that high scores of knowledge, attitude, and behavior were only found in 33%, 32% and 27% respectively and the higher score of knowledge was associated with place of residence, being familiar with the non-close person with mental illness, and younger age less than 70 years, whereas having a high level of education, being familiar with close people with mental illness was associated with less stigmatizing behavior, which is consistent with our findings regarding contact with mentally ill in the last 3 months as a predictor in a change in attitude [20]. in another study done in Buenos Aires in Argentina 2018 to study the reported and intended behavior towards people with mental health problems using RIBS and included a large sample of 1156 patients, most of the respondents reported a high level of willingness to interact with people with mental health problems, this tendency was found mainly among the respondents younger than 40 years old, and with higher education; level and who had the previous relationship with people with mental problems. The findings of the last study confirm the findings of the previous study and denote that the findings of our study with undergraduate medical study may be even higher than the general population [21].
Limitations of the study
The main limitations of this study are common in all survey studies that depend on recall of information and are subject to many sorts of biases including, the tendency to average, tendency polarity, agreeing with statements without thinking, and others. Qualitative methods like the use of a non-structured questionnaire and thematic analysis may be another useful methodology.
In this study, pre-final undergraduate medical students showed little poor mental health-related knowledge, and poor stigmatizing beliefs and behavior, towards mentally ill patients. More efforts are needed to improve the knowledge, challenge and reverse stigmatizing beliefs, and attitudes, of undergraduate medical students towards mentally ill patients and more studies are needed to measure the outcomes of anti-stigma educational interventions.
Declaration
- The Ethical Committee of the faculty of medicine, Suez Canal University had given its approval for conducting the study before the recruitment of the first participant.
- Consent to participate in the study was obtained from all the study participants, and prior to their enrollment in the study.
- Consent for publication of the study was approved by the Department of family medicine, Suez Canal University.
- The data of the study is available publically in both Excel sheets and SPSS data form.
- No conflict of interest is worth to be mentioned.
- No funding was offered to carry out this study.
- The authors of this study are all faculty staff members, of Suez Canal University, known for their significant contributions to establishing and promoting, Family Medicine specialty, since the inception of the faculty of medicine, Suez Canal University, was the first Faculty of medicine in Egypt, adopting, community-oriented education, and establishing the first academic department in the Middle East for Primary Care, and Family medicine. They all participated in the Health Reform Project carried out in Egypt, helped to establish many family medicine departments in the country, and successfully helped establish” The Egyptian Board of Family Medicine”, as a distinct clinical specialty.
Special thanks are due to Dr. Menna M Saad, for the great effort, she done, in every step of this work until its completion.
- Thornicroft G. Physical health disparities and mental illness: the scandal of premature mortality. Br J Psychiatry. 2011 Dec;199(6):441-2. doi: 10.1192/bjp.bp.111.092718. PMID: 22130744.
- World health organization. Mental health day: mental disorders. 2018. http://www.who.int/news-room/fact-sheets/detail/mental-disorders.
- Disability Rights Commission, equal treatment: Closing the Gap. A Formal Investigation into Physical Health Inequalities experienced by people with learning disabilities and mental health problems. 2006.
- Lauber C, Anthony M, Ajdacic-Gross V, Rössler W. What about psychiatrists' attitude to mentally ill people? Eur Psychiatry. 2004 Nov;19(7):423-7. doi: 10.1016/j.eurpsy.2004.06.019. PMID: 15504649.
- Kassam A, Glozier N, Leese M, Loughran J, Thornicroft G. A controlled trial of mental illness related stigma training for medical students. BMC Med Educ. 2011 Jul 29;11:51. doi: 10.1186/1472-6920-11-51. PMID: 21801355; PMCID: PMC3161004.
- Luty J, Fekadu D, Umoh O, Gallagher J. Validation of a short instrument to measure stigmatized attitudes towards mental illness. Psychiatry Bull. 2006; 30:257-260.
- Pintard PJ, Sciascia S. Medical students’ attitudes about mental illness. Psychiatry Serv. 2012; 63:836.
- Ucok A, Polat A, Sartorius N, Erkoc S, Atakli C. Attitudes of psychiatrists towards schizophrenia. Psychiatry Clinic Neuroscience. 2014; 58:89–91.
- Shahrour TM, Rehmani RS. Testing psychiatric stigma in a general hospital in Saudi Arabia. Saudi Med J. 2009 Oct;30(10):1336-9. PMID: 19838444.
- Evans-Lacko S, Henderson C, Thornicroft G. Public knowledge, attitudes and behaviour regarding people with mental illness in England 2009-2012. Br J Psychiatry Suppl. 2013 Apr;55:s51-7. doi: 10.1192/bjp.bp.112.112979. PMID: 23553695.
- Evans-Lacko S, Little K, Meltzer H, Rose D, Rhydderch D, Henderson C, Thornicroft G. Development and psychometric properties of the Mental Health Knowledge Schedule. Can J Psychiatry. 2010 Jul;55(7):440-8. doi: 10.1177/070674371005500707. PMID: 20704771.
- Hirai M, Clum GA. Development, Reliability, and Validity of the Beliefs Toward mental Illness Scale. Journal pf psychopathology and Behavioral Assessment. 2000; 22: 221-236.
- Evans-Lacko S, Rose D, Little K, Flach C, Rhydderch D, Henderson C, Thornicroft G. Development and psychometric properties of the reported and intended behaviour scale (RIBS): a stigma-related behaviour measure. Epidemiol Psychiatr Sci. 2011 Sep;20(3):263-71. doi: 10.1017/s2045796011000308. PMID: 21922969.
- Chawla JM, Balhara YP, Sagar R, Shivaprakash. Undergraduate medical students' attitude toward psychiatry: a cross-sectional study. Indian J Psychiatry. 2012 Jan;54(1):37-40. doi: 10.4103/0019-5545.94643. PMID: 22556435; PMCID: PMC3339216.
- James BO, Omoaregba JO, Okogbenin EO. Stigmatising attitudes towards persons with mental illness: a survey of medical students and interns from southern Nigeria. Ment Illn. 2012 Apr 30;4(1):e8. doi: 10.4081/mi.2012.e8. PMID: 25478110; PMCID: PMC4253366.
- Poreddi V, Thimmaiah R, Math SB. Attitudes toward people with mental illness among medical students. J Neurosci Rural Pract. 2015 Jul-Sep;6(3):349-54. doi: 10.4103/0976-3147.154564. PMID: 26167018; PMCID: PMC4481789.
- Altindag A. Effects of an anti-stigma program on medical students’ attitudes towards people with schizophrenia. Psychiatry Clinic Neuro-Science. 2006; 60(3):283–288.
- Alaa El-Din MA. Attitude of medical students toward mentally ill patients: impact of a clinical psychiatric round. The Egyptian Journal of Neurology, Psychiatry and Neurosurgery. 2016; 53(1):6–11.
- Hearn J, Marwood M. Evaluating mental health literacy in medical students in the United Kingdom. Journal of Mental Health Training. 2019; 14(5):339-347. doi: 10.1108/JMHTEP-01-2019-0001
- Abi Doumit C, Haddad C, Sacre H, Salameh P, Akel M, Obeid S, Akiki M, Mattar E, Hilal N, Hallit S, Soufia M. Knowledge, attitude and behaviors towards patients with mental illness: Results from a national Lebanese study. PLoS One. 2019 Sep 16;14(9):e0222172. doi: 10.1371/journal.pone.0222172. PMID: 31525219; PMCID: PMC6746362.
- Zalazar V. Reported and intended behavior towards people with mental health problem in Argentina, International Journal of Mental Health. 2018; 47:3215-227