More Information
Submitted: August 12, 2022 | Approved: September 28, 2022 | Published: September 29, 2022
How to cite this article: Gultekin N. Idiopathic progressive polyneuropathy presented with frequently acute pulmonary oedema: a case report. J Neurosci Neurol Disord. 2022; 6: 045-048.
DOI: 10.29328/journal.jnnd.1001068
Copyright License: © 2022 Gultekin N. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Polyneuropathy; Acute pulmonary edema; Prednisolone; ACTH
Idiopathic progressive polyneuropathy presented with frequently acute pulmonary oedema: a case report
Nazmi Gultekin*
Cardiology Institute, İstanbul University, Istanbul, Turkey
*Address for Correspondence: Dr. Nazmi Gultekin, Professor, Cardiology Institute, Istanbul University, Istanbul, Turkey, Email: [email protected]
Neuropathy is when nerve damage interferes with the functioning of the peripheral nervous system (PNS). When the cause can’t be determined, it’s called idiopathic neuropathy(Idiopathic neuropathy, now designated as chronic idiopathic axonal polyneuropathy (CIAP).
There are three kinds of nerves within the PNS. Sensory nerves relay messages from the sense organs to the brain. This allows sensations of temperature and touch. Motor nerves transmit signals from the brain to the muscles. This helps the brain control the muscles. Autonomic nerves control body functions like heart rate, breathing, and digestion.
Damage to nerve cells can affect how the PNS communicates with the rest of the body. Symptoms can include numbness, pain, and balance issues.
It’s called acute neuropathy when symptoms develop suddenly. Alternately, it’s called chronic neuropathy when symptoms start slowly and increase over time. Diagnosis involves physical examination and review of medical history. Diagnostic testing may include blood tests, nerve testing, and imaging tests.
There is no cure for idiopathic neuropathy. Treatments including medication, physical therapy, and lifestyle modifications can help you function and feel better.
We report a case of idiopathic polyneuropathy presented with frequent acute pulmonary edema for a year.
Many causes of Noncardiogenic Pulmonary Edema (NPE) exist including the following: drowning, acute glomerul-onephritis, fluid overload, aspiration, inhalation injury, neurogenic pulmonary edema, allergic reaction, adult respiratory distress syndrome (ARDS) [1,2]. Two major components contribute to the pathogenesis of NPE: elevated intravascular pressure and pulmonary capillary leak. Therefore, hemodynamic cardiogenic and noncardiogenic components exist.
These components often work in concert, as in pulmonary edema after epileptic convulsions or intracranial pressure elevation. The hemodynamic component is relatively brief and may unmask pure NPE, such as that seen in experimental seizures. An initial and rapid increase in pulmonary vascular pressure due to pulmonary vasoconstriction or pulmonary blood flow can lead to pulmonary microvascular injury [3]. An increase in vascular permeability consequently results in edema formation, as suggested by the frequent observation of pulmonary hemorrhage in NPE (i.e., the blast theory) (Table 1). In order to avoid life-threatening complications, prompt recognition of NPE is important. The use of a chest roentgenogram and other tests is key to establishing the diagnosis and to distinguishing between the 2 types of pulmonary edema. The correct diagnosis relies on clinical and radiologic findings, despite some overlap in the clinical and imaging findings between the different causes [1-3].
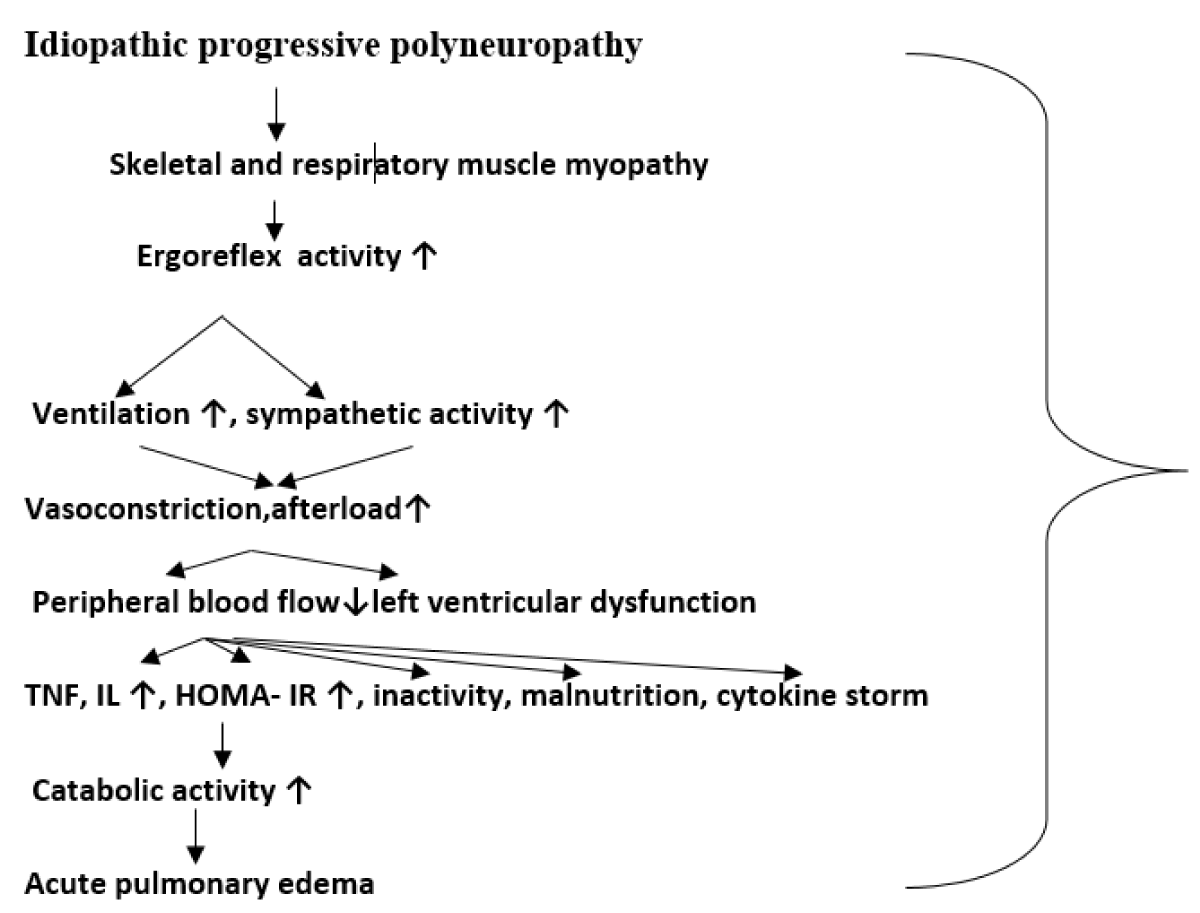
Table 1: Polyneuropathy & acute pulmonary edema connection.
Most patients with NPE are seriously ill and immobile. Conventional chest roentgenogram is readily and universally available, and it has the added advantage of portability; chest roentgenograms are the examination of choice [4-7].
In conjunction with the clinical presentation, radiographic findings are generally sufficient to arrive at a diagnosis of NPE and preferred examination. Gadolinium-based magnetic resonance imaging (MRI) contrast agents have been associated with several adverse effects, some of which can be serious. It has extremely rare life-threatening systemic complications, which can lead to bronchospasm, hypersensitivity reactions, and cardiovascular arrest [8].
Chronic idiopathic sensory-motor polyneuropathy is a frequent neurologic disorder in elderly persons [6]. Idiopathic polyneuropathy is a sensory and motor nerve damage, that affects functions of the peripheral nervous system and mostly the cause can not clearly be found [4-7]. In addition to paresthesias, numbness, and pain in the hand, feet, and junctional muscles, respiratory muscles are also affected by neuromuscular diseases [9].
We report a case of idiopathic polyneuropathy presented with frequent acute pulmonary edema for a year. A 90-years –old female patient followed for years with idiopathic progressive polyneuropathy accompanied by countless times of acute pulmonary edema (approximately 30-40 times) was admitted to the emergency department with extreme breathlessness and excessive anxiety.
She had a history of diabetes mellitus and coronary artery disease In this patient’s last coronary angiography, LMCA was normal. LAD ostium was 30% - 40% stenosis, proximal stent open, no feature. No feature other than wall irregularity except in CX ostium atheroma plaque available. There was 70% - 80% stenosis in the moderately developed proximal of OM1. No features except CXPL and CXPD wall irregularities. In non-dominant RCA was wall irregularity. 2.25 X 18 mm Resolute stent was inserted into CXOM1. She was medicated with conventional heart failure treatment (100 mg/day aspirin, metoprolol 50 mg twice daily, Apixaban 2.5 mg twice daily, 40 mg furosemide digoxin 1.25 mg/daily 5 days a week, and clopidogrel 75 mg once a daily). In addition, this patient was being followed up with the diagnosis of idiopathic polyneuropathy by Istanbul University Neurology Clinic for many years and was receiving maintenance treatment with gabapentin 900 mg and methylprednisolone 4 mg/day. Clinical examination findings such as numbness, tingling, muscle weakness, and weight loss; electrophysiological and nerve biopsy studies were consistent with chronic idiopathic axonal polyneuropathy.
At the last admission, the physical examination revealed rales and rhonchi bilaterally and pink, frothy sputum, and orthopnea were seen. Her chest graph showed bilaterally pulmonary infiltrates compatible with pulmonary edema. Her blood pressure was 115/65 mmHg and her heart rate was 100 beats per minute with an irregular rhythm. The presenting ECG revealed atrial fibrillation in all leads. Transthoracic echocardiography showed an apical segment of the left ventricle was aneurismatic. The estimated left ventricular ejection fraction was 40%. On admission, laboratory results were as follows:
Serum creatinine 2.9 mg/dl, BUN 26, hs-cTnT 28 ng/l, BNP 325 pg/ml,CRP 93.11 mg/l(0-5), hematocrit 25.9%, hemoglobin 9.3 g/dl, Na 121 mEq/L, K 3.8 mEq/L calcium 8.6 mg/dl. Arterial blood gas analysis showed a pH of 7.487, a pCO2 of 40,9 mmHg, pO2 of 51.9 mmHg, and O2 saturation of 85.8%. CVP of the patient was 8 mm Hg, PWCP 10 mm Hg.
The volume status of the patient was about 2100 ml daily intake and 2000 ml daily urine output on days before hospitalization.
The patient was admitted to the intensive care unit. Furosemide at 125 mg/minute and renal dose dopamine as 200 microgram/minute infusion were administered. The patient did not respond to treatment. Also, she was medicated with conventional heart failure treatment (100 mg/day aspirin, metoprolol 50 mg twice daily, Apixaban 2.5 mg twice daily).
But the hemodynamic status of the patient deteriorated due to certain symptoms similar to the aging-related essential tremor that were tremors in jaws and hands all peripheral and respiratory muscle weakness. In addition, this patient with orthopnea and unexplained shortness of breath should be considered in terms of diaphragm dysfunction due to phrenic neuropathy. Thus, we thought to investigate whether Idiopathic Progressive Polyneuropathy could play a role in the development of pulmonary edema countless times by measuring inspiratory and expiratory muscle strength. Therefore, Maximal expiratory pressure (MEP) and maximal inspiratory pressure (MIP) were examined by physiotherapists; there found 34 and 27 cm H2O respectively.
Continuous positive airway pressure therapy(CPAP), O2 therapy, and inhaler agents were performed in case of dyspnea. Prednisolone and adrenocorticotropic hormone, flecainide 100 mg once daily were added in current treatments. Valsartan + sacubitril 24/26 mg twice daily was added after the patient was stabilized. The patient’s clinical status and peripheral muscles including respiratory muscles were improved, on the other hand in this patient, Bun 24 mg/dl, creatinine, 0.92 mg/dl, po2 101 mm Hg, pCo2 35.2 mm Hg was detected upon discharge from the hospital, and still doing well for one three years follow up.
We have reported a case of idiopathic polyneuropathy presented with frequent acute pulmonary edema for a year. Idiopathic polyneuropathy is a sensory and motor nerve damage, that affects functions of the peripheral nervous system and mostly the cause can not clearly be found. The most common cause is diabetes. Other common causes include alcohol abuse, poor nutrition, autoimmune processes (where the body’s own immune system attacks parts of the nerves), and genes. Exposure to certain drugs or toxins can lead to neuropathy. Demirhan et al describe a case of noncardiogenic pulmonary edema associated with the contrast in a 37-year-old man reported after an intravenous injection of gadobutrol during MRI [4-9].
Direct pressure or compression of a single nerve—like in carpal tunnel syndrome—may cause it to malfunction.
As known; carpal tunnel syndrome is caused by pressure on the median nerve. It provides sensation to the palm side of your thumb and fingers, except the little finger. It also provides nerve signals to move the muscles around the base of your thumb (motor function [10]).
However, Chronic idiopathic axonal polyneuropathy (CIAP) is a term describing neuropathies with both sensory and motor involvement in a length-dependent distribution where neurophysiology reveals axonal damage, neuropathy onset is insidious and shows slow or no progression of the disease over at least 6 months with no etiology being identified despite appropriate investigations.
CIAP may cause numbness, tingling, and weakness. It can also cause pain. These symptoms usually start in the longest nerves in the body and so first affect the feet and later the hands. This is sometimes called the “stocking-glove” pattern. The symptoms usually spread slowly and evenly up the legs and arms. Other body parts might also be affected. Most people who develop peripheral neuropathy are over age 55. But people can be affected at any age. In addition to paresthesias, numbness, and pain in the hand, feet, and junctional muscles, respiratory muscles are also affected by CİAP [4-9].
There are two fundamentally different types of pulmonary edema; cardiogenic and non-cardiogenic.
Cardiogenic pulmonary edema is classically treated with afterload reduction although non-cardiogenic pulmonary edema requires respiratory support with low tidal volume and low dose hydrocortisone. Neuropathy of respiratory muscles and phrenic nerves is a major cause of dyspnea and hypercapnic respiratory failure [1-3]. MEP/MIP presents phrenic and respiratory muscle neuropathy and also relieves estimated information about the pulmonary function that can be used in patients who cannot tolerate pulmonary function tests but not certainly differentiate from cardiogenic pulmonary edema [11]. MEP and MIP were examined by a physiotherapist and were determined as 34 and 27 cm H2O respectively in the patient. (MIP: must be > 60 cm H2O or over) (for 65 - 85 years old female), and down - 30 cm H2O is accompanied by severe respiratory distress. MEP: > 40 cm H2O (for 65 - 85 years old female). MEP: must be > positive, 40 cm H2O and coughing strain and secretion is accompanied by when 40 cm H2O is low). Therefore, continuous positive airway pressure therapy was performed in case of dyspnea [12]. Prednisolone 40 mg/day and adrenocorticotropic hormone 1 mg every other day were added to existing treatments (combined with prednisolone) [1-3]. Then, valsartan + sacubitril 24/26 mg was added after the patient was stabilized. The patient’s clinical status and peripheral muscles including respiratory muscles were improved (MIP, 30 cm H2O; MEP: positive, 36 cm H2O). This patient was doing well during three years of follow-up. However, we recently learned that this patient died after intubation in another hospital with a similar picture.
Idiopathic polyneuropathy is a sensory and motor nerve damage, that affects functions of the peripheral nervous system and mostly the cause can not clearly be found. Cardiogenic pulmonary edema is classically treated with afterload reduction although non-cardiogenic pulmonary edema requires respiratory support with low tidal volume, low dose hydrocortisone, and adrenocorticotropic hormone(ACTH). Neuropathy of respiratory muscles and phrenic nerves is a major cause of dyspnea and hypercapnic respiratory failure. MEP/MIP presents phrenic and respiratory muscle neuropathy and also relieves estimated information about the pulmonary function that can be used in patients who cannot tolerate pulmonary function tests but not certainly differentiate from cardiogenic pulmonary edema. Intubation should be avoided in patients with CIAP unless it is absolutely necessary. We think that continuous positive airway pressure therapy is more appropriate than unnecessary intubation.
- Ware LB, Matthay MA. Clinical practice. Acute pulmonary edema. N Engl J Med. 2005 Dec 29;353(26):2788-96. doi: 10.1056/NEJMcp052699. PMID: 16382065.
- O'Leary, R.; McKinlay, J. (2011). "Neurogenic pulmonary oedema". Continuing Education in Anaesthesia, Critical Care & Pain. 11 (3): 87–92. doi:10.1093/bjaceaccp/mkr006.
- Givertz MM, Gottlieb SS, Finlay G. Noncardiogenic pulmonary edema. https://www.uptodate.com/contents/noncardiogenic-pulmonary-edema.Feb 6, 2018.
- What is peripheral neuropathy. The Foundation for Peripheral Neuropathy. https://www.foundationforpn.org/what-is-peripheral-neuropathy/. Accessed April 2, 2016.
- Rutkove SB. Overview of polyneuropathy. http://www.uptodate.com/home. Accessed April 2, 2016.
- Vrancken AF, Franssen H, Wokke JH, Teunissen LL, Notermans NC. Chronic idiopathic axonal polyneuropathy and successful aging of the peripheral nervous system in elderly people. Arch Neurol. 2002 Apr;59(4):533-40. doi: 10.1001/archneur.59.4.533. PMID: 11939887.
- Visser NA, Vrancken AF, van der Schouw YT, van den Berg LH, Notermans NC. Chronic idiopathic axonal polyneuropathy is associated with the metabolic syndrome. Diabetes Care. 2013 Apr;36(4):817-22. doi: 10.2337/dc12-0469. Epub 2012 Nov 30. PMID: 23204246; PMCID: PMC3609524.
- Demirhan A, Yasar Tekelioglu U, Akkaya A, Dagistan E, Suzi Ayhan S, Ozturk S, Yildiz I, Kocoglu H. Magnetic resonance imaging contrast agent related pulmonary edema: a case report. Eur Rev Med Pharmacol Sci. 2012 Oct;16 Suppl 4:110-2. PMID: 23090824.
- Sprooten RTM, Otte AAB, Cobben NAM, Steijns SCM, Rohde GGU, Wouters EFM. Orthopnea due to phrenic nerve involvement in neuralgic amyothrophy. European Respiratory Journal. 2014 44: P452.
- Burton C, Chesterton LS, Davenport G. Diagnosing and managing carpal tunnel syndrome in primary care. Br J Gen Pract. 2014 May;64(622):262-3. doi: 10.3399/bjgp14X679903. PMID: 24771836; PMCID: PMC4001168.
- Cahalin LP, Arena R, Guazzi M, Myers J, Cipriano G, Chiappa G, Lavie CJ, Forman DE. Inspiratory muscle training in heart disease and heart failure: a review of the literature with a focus on method of training and outcomes. Expert Rev Cardiovasc Ther. 2013 Feb;11(2):161-77. doi: 10.1586/erc.12.191. Erratum in: Expert Rev Cardiovasc Ther. 2013 Apr;11(4):520. PMID: 23405838; PMCID: PMC7304053.
- Berbenetz N, Wang Y, Brown J, Godfrey C, Ahmad M, Vital FM, Lambiase P, Banerjee A, Bakhai A, Chong M. Non-invasive positive pressure ventilation (CPAP or bilevel NPPV) for cardiogenic pulmonary oedema. Cochrane Database Syst Rev. 2019 Apr 5;4(4):CD005351. doi: 10.1002/14651858.CD005351.pub4. PMID: 30950507; PMCID: PMC6449889.