More Information
Submitted: October 31, 2022 | Approved: November 10, 2022 | Published: November 11, 2022
How to cite this article: Lizzeik D, Ibrahim C, Shatila AR. Pseudomonas stutzeri meningitis in a patient with post-laminectomy CSF leak and infected pseudomeningocele: a case report. J Neurosci Neurol Disord. 2022; 6: 072-075.
DOI: 10.29328/journal.jnnd.1001071
Copyright License: © 2022 Lizzeik D, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Pseudomonas stutzeri meningitis in a patient with post-laminectomy CSF leak and infected pseudomeningocele: a case report
Dina Lizzeik1,2*, Christelle Ibrahim1,2 and Abdul Rahman Shatila1,2
1Gilbert and Rose-Marie Chagoury School of Medicine, Lebanese American University, Byblos, Lebanon
2Department of Neurology, Lebanese American University Medical Center-Rizk Hospital, Beirut, Lebanon
*Address for Correspondence: Dina Lizzeik, Gilbert and Rose-Marie Chagoury School of Medicine, Lebanese American University, Byblos, Lebanon, Email: [email protected]
Spine degenerative surgeries are very common but carry multiple complications such as dural tears, CSF leak, pseudomeningocele and very rarely meningitis. Here we report such a case and discuss the possible causes, management and review of the literature.
It’s a case of a 68-year-old man who underwent a posterior laminectomy that was complicated by a CSF leak and pseudomeningocele. Twelve days later the patient developed a severe bifrontal headache and then altered sensorium. CSF studies revealed severe meningitis with Pseudomonas stutzeri. It was multi-sensitive and after initiation of gram-negative coverage the patient markedly improved. However, the meningitis was further complicated by cerebral venous sinus thrombosis and he was also started on anticoagulation.
Conclusion: Pseudomonas stutzeri has rarely been reported as a cause of meningitis and has never been reported post-laminectomy. Meningitis symptoms and signs could be obscured by the use of steroids in the postoperative period. Hence, it is of paramount importance to look for any subtle signs of infection in the postoperative period and question the use of high-dose steroids that could easily mask them.
Post-laminectomy dural tear carries an incidence ranging between 0.2% and 20% [1]. It has been associated with surgical site infection for varied reasons related to prolonged surgical time, the formation of a CSF fluid collection with a possible fistula and the prolonged bed rest associated with conservative management of surgical dural tears [1].
Usually, these tears are easily detected by the surgeon and managed intraoperatively, either through direct suturing with or without the use of fibrin glue or with the application of muscle or fat graft to cover the area of the tear [2]. In other instances, they are left untreated and risk other more serious complications like CSF fistula formation, pseudomeningocele, meningitis, arachnoiditis and epidural abscess [3]. The incidence of pseudomeningocele ranges between 0.068% and 2% [4] and that of meningitis 0.10 % [5].
In this paper, we report a case of meningitis with an opportunistic bacterium secondary to a CSF leak and venous sinus thrombosis post-laminectomy. Pseudomonas stutzeri is a very rare cause of meningitis [6-9]. It has never been reported post-laminectomy surgery.
This is the case of a 68-year-old man known to have hypertension, dyslipidemia and glaucoma who presented to our hospital with symptoms of L5 radiculopathy of 2 weeks duration. The patient had intractable pain mostly in the lateral aspect of the right thigh radiating up to the right big. On exam, the patient had a mild weakness (4/5 MRC), of right foot inversion and dorsiflexion.
MRI showed a right posterolateral fragmented herniation of the disc at L3/L4 with large extruded fragments extending inferiorly in the right recess behind the upper two-thirds of L4, moderately narrowing the recess and compressing the right L4 nerve root.
The patient underwent discectomy 3 days after hospitalization, during which he received a combination of paracetamol, tramadol, pregabalin and Solu-Medrol 120 mg intravenous daily as part of his pain management. Post-operatively, the patient had significant relief from his pain. A surgical drain was inserted and up to one week, it was still draining clear fluid suggestive of a CSF leak secondary to a dural tear. After the drain removal, a copious amount of clear fluid was still leaking through the surgical incision. The patient was started on acetazolamide 500 mg twice daily and hydration. He was discharged post-op day 6 on acetazolamide, Coenzyme Q10, magnesium and pregabalin, paracetamol and tramadol as needed for severe pain. Steroids were discontinued.
The patient was readmitted 3 days later (post-op day 9) with severe right lateral and posterior lower leg pain exacerbated by the Valsalva maneuver and relieved by certain postures and analgesics. The patient was continued on the previously mentioned medications, and high-dose steroids were restarted for disc-related radicular pain.
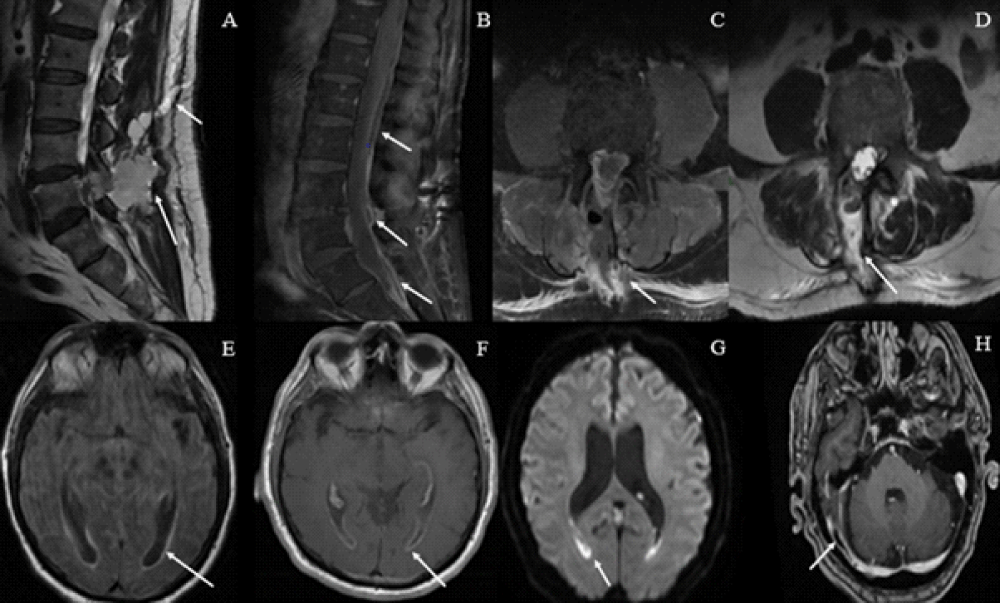
An MRI of the lumbosacral spine with gadolinium is shown in (Figure 1A). Findings were suggestive of a post-operative seroma with possible associated CSF leak.
Three days after the second admission (post-op day 12) the patient developed a new severe bifrontal headache and severe lower back pain. Bacterial culture from the surgical wound revealed coagulase-negative Staphylococcus and the patient was started on Vancomycin and Rifampin.
The headache became worse with protracted vomiting, a depressed mental state, and severe neck stiffness. An urgent NCCT brain was unremarkable but the MRI of the brain demonstrated signs of ventriculitis as shown in (Figure 1B). The MRV did not show sinus thrombosis. The patient was started on Meropenem for possible meningitis. The failure of leptomeningeal enhancement was attributed to steroids.
Figure 1: A) Day 6 post-op: MRI lumbosacral spine with gadolinium showing a collection at the surgical bed measuring 16 x 39 x 53 mm non-enhancing (see arrow), seen posteriorly communicating with a similar subcutaneous fluid collection measuring 17 x 30 x 60 mm that communicates with the skin (see arrow) B) 4 weeks post op: MRI lumbosacral spine showed 3 focal posterior epidural collections with rim enhancement suggestive of epidural abscesses (see arrow). C and D) 5 x 2 cm rim enhancing fluid collection suggestive of infected post-operative seroma (see arrow). E) Day 9 post-op: MRI of the brain with gadolinium showed mild ventriculomegaly with abnormal signal along the inner lining of the occipital horns of lateral ventricles suggestive of ventriculitis with diffuse gyral intermediate signal on FLAIR without corresponding leptomeningeal enhancement or bleed (see arrow). F) 4 weeks post-op: MRI brain with gadolinium demonstrating post-contrast enhancement consistent with ventriculitis (see arrow) G) diffusion restriction of the ventricular lining at the temporal horn of the lateral ventricles bilaterally on DWI imaging (see arrow). Findings are consistent with ventriculitis. H) Also demonstrated subacute right sigmoid and right transverse sinus thrombosis (see arrow).
A lumbar puncture was done (on post-op day 15) and showed a CSF white cell count of 50 000/mm3 with 0 glucose and 755 mg/dl protein. Amikacin was added to Meropenem and Vancomycin. Steroids were discontinued. EEG showed moderate background slowing without epileptiform discharges.
It is noted that during the admission the patient did not have a change in his white blood cell count (the first rise with neutrophilia was attributed to steroid use) and no change in serum CRP level as displayed in Table 1.
| Table 1: relevant laboratory workup demonstrating a suppression in the rise of inflammatory markers when on high dose steroids and the rise in WBC count at day 3 attributable to steroids use, with the CSF studies at day 9. | |||
| Day 6 post-op | Day 9 post-op | Day 15 post-op | |
| White blood cell count (x10³/µL) | 9.37 | 20.36 | 23.64 |
| Neutrophil count (%) | 69.4 | 86 | 94.6 |
| CRP (mg/dL) | 0.5 | 0.2 | 27.8 |
| CSF studies | |||
| Appearance | Turbid | ||
| WBC (/mm3) | 52500 | ||
| RBC (/mm3) | 200 | ||
| Neutrophils (%) | 100% | ||
| Glucose (mg/dL) | <5 | ||
| Protein (mg/dL) | 755 | ||
The patient showed marked improvement, both clinically and laboratory. He was coherent and cooperative with normal neurological examination except for neck stiffness.
A repeat MRI lumbosacral spine with gadolinium revealed near complete resolution of CSF collection, with no evident filling defect to suggest a CSF leak.
Bacterial cultures revealed multi-sensitive Pseudomonas stutzeri and the antibiotic regimen was de-escalated to ciprofloxacin and piperacillin/tazobactam, later switched to ceftriaxone and ciprofloxacin.
A repeat MRI brain and MRI of the lumbosacral spine with gadolinium 2 weeks later is shown in (Figure 1C-H). Accordingly, the patient was started on rivaroxaban and CT-guided needle aspiration of the collection showed negative culture.
The patient improved markedly with complete resolution of the headache, and neck stiffness and was fully ambulatory without back pain. He was discharged on Ciprofloxacin 500 mg bid for three more weeks.
Bacterial meningitis post-spinal surgery is a very rare complication, reported in the literature to be 0.1% [5] and is associated with poor prognosis. The diagnosis of meningitis may be delayed several days because of the administration of pain medication and sometimes steroids leading to increased morbidity. The common organisms associated with post-operative meningitis are Staphylococcus aureus, Acinetobacter and Pseudomonas aeruginosa [10]. Post-laminectomy meningitis with Pseudomonas stutzeri has never been reported to our knowledge.
Pseudomeningocele is also quite a rare post-spinal surgery, in which a durotomy with concomitant arachnoid tear leads to one-way CSF flow to the extradural space resulting in a false cyst formation [4]. They occur more commonly in the lumbar region due to the higher hydrostatic pressure that the CSF exists in the lumbar spine and due to the fact that lumbar surgery is more common than cervical or thoracic spine surgeries [4]. They can remain asymptomatic and thus the optimal management of these cysts is controversial [4]. It is preferred to manage asymptomatic pseudomeningocele conservatively since even large pseudomeningocele were seen to scale down with time [11]. However, they can sometimes result in varied symptoms from mild headache, nausea and vomiting, radicular pain to infection [4]. Meningitis has rarely been reported with pseudomeningocele and one report of MRI findings includes bony erosions [12]. The surgical management of pseudomeningocele has been described in detail by Weng, et al. [11]. In our patient, Pseudomonas stutzeri meningitis occurred after the pseudomeningocele was infected with the organism and through a persistent fistula tract caused fulminant meningitis. We suspect that the sudden onset of severe headache and neck stiffness with worsening mental state was related to the infected cyst rupture into the subarachnoid space causing the rapid deterioration.
Pseudomonas stutzeri is a rare cause of nosocomial infections. It is an aerobic, gram-negative bacteria [13], found in soil and water and is usually considered a colonizer or a contaminant [8]. It has been reported as a rare cause of meningitis. It was reported as community-acquired meningitis in an immunocompromised patient [7] and as a nosocomial infection in a neurosurgery patient related to contaminated subdural grid electrodes [8] and an indolent cause of meningitis in two neurosurgery patients 2 years after their surgery [6]. The organism has low virulence with high susceptibility to fluoroquinolones, aminoglycosides, 3rd generation cephalosporins, and carbapenems [9]. This explains the rapid response in our patients to high-dose combination antibiotic therapy.
It is possible that our patient contracted the organism either intraoperatively or through an infected surgical incision from colonized skin, or through an IV route with bacteremia and secondary pseudomeningocele infection.
Durotomy is not uncommon post-laminectomy and careful monitoring for possible complications is mandatory. The role of steroids in the postoperative period is controversial and their use should be assessed on a risk-benefit analysis. Steroids can mask a subclinical infection and may delay the diagnosis of meningitis as in our case. If steroids are used then a close follow-up with serial markers of infection such as CBCD, ESR and CRP as well as procalcitonin should be done.
- Takenaka S, Makino T, Sakai Y, Kashii M, Iwasaki M, Yoshikawa H, Kaito T. Dural tear is associated with an increased rate of other perioperative complications in primary lumbar spine surgery for degenerative diseases. Medicine (Baltimore). 2019 Jan;98(1):e13970. doi: 10.1097/MD.0000000000013970. PMID: 30608436; PMCID: PMC6344202.
- Papadakis M, Aggeliki L, Papadopoulos EC, Girardi FP. Common surgical complications in degenerative spinal surgery. World J Orthop. 2013 Apr 18;4(2):62-6. doi: 10.5312/wjo.v4.i2.62. PMID: 23610753; PMCID: PMC3631953.
- Kalevski SK, Peev NA, Haritonov DG. Incidental Dural Tears in lumbar decompressive surgery: Incidence, causes, treatment, results. Asian J Neurosurg. 2010 Jan;5(1):54-9. PMID: 22028744; PMCID: PMC3198662.
- Viswanathan VK. Pseudomeningocele after spine surgery: An important cause for failed back syndrome and its management–a mini review. MOJ Surgery 2018; 6. doi:10.15406/mojs.2018.06.00132
- Lin TY, Chen WJ, Hsieh MK, Lu ML, Tsai TT, Lai PL, Fu TS, Niu CC, Chen LH. Postoperative meningitis after spinal surgery: a review of 21 cases from 20,178 patients. BMC Infect Dis. 2014 Apr 23;14:220. doi: 10.1186/1471-2334-14-220. PMID: 24755138; PMCID: PMC4013809.
- Ma BT, Anuta M, Ferrer P. Pseudomonas stutzeri infection presenting as delayed-onset adult bacterial meningitis in two post-neurosurgery patients: A case report. J Neurol Sci 2019; 405:112. doi:10.1016/j.jns.2019.10.1781
- Roig P, Orti A, Navarro V. Meningitis due to Pseudomonas stutzeri in a patient infected with human immunodeficiency virus. Clin Infect Dis. 1996 Mar;22(3):587-8. doi: 10.1093/clinids/22.3.587. PMID: 8852995.
- Yee-Guardino S, Danziger-Isakov L, Knouse M, Bingaman W, Sabella C, Goldfarb J. Nosocomially acquired Pseudomonas stutzeri brain abscess in a child: case report and review. Infect Control Hosp Epidemiol. 2006 Jun;27(6):630-2. doi: 10.1086/504935. Epub 2006 May 17. PMID: 16755486.
- Lalucat J, Bennasar A, Bosch R, García-Valdés E, Palleroni NJ. Biology of Pseudomonas stutzeri. Microbiol Mol Biol Rev. 2006 Jun;70(2):510-47. doi: 10.1128/MMBR.00047-05. PMID: 16760312; PMCID: PMC1489536.
- Zhou H, Zhang X. Intracranial malignant lesions correlate with the requirement for a long treatment course in postoperative central nervous system infection. Neuropsychiatr Dis Treat. 2014 Nov 4;10:2071-7. doi: 10.2147/NDT.S71836. PMID: 25395855; PMCID: PMC4226452.
- Weng YJ, Cheng CC, Li YY, Huang TJ, Hsu RW. Management of giant pseudomeningoceles after spinal surgery. BMC Musculoskelet Disord. 2010 Mar 21;11:53. doi: 10.1186/1471-2474-11-53. PMID: 20302667; PMCID: PMC2848136.
- Radcliff K, Morrison WB, Kepler C, Moore J, Sidhu GS, Gendelberg D, Miller L, Sonagli MA, Vaccaro AR. Distinguishing Pseudomeningocele, Epidural Hematoma, and Postoperative Infection on Postoperative MRI. Clin Spine Surg. 2016 Nov;29(9):E471-E474. doi: 10.1097/BSD.0b013e31828f9203. PMID: 27755204.
- Bisharat N, Gorlachev T, Keness Y. 0-Years Hospital Experience in Pseudomonas stutzeri and Literature Review. 2012.