More Information
Submitted: September 21, 2023 | Approved: September 28, 2023 | Published: September 29, 2023
How to cite this article: Siriguppa N, Prem Kumar BN. Effect of Balance Exercises with Smart Phone Based Virtual Reality Programme on Balance in Stroke Patients. J Neurosci Neurol Disord. 2023; 7: 104-112.
DOI: 10.29328/journal.jnnd.1001084
Copyright License: © 2023 Siriguppa N, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Postural control; Balance; Stroke; Perturbation-based balance training; Smartphone-based virtual reality; Virtual reality balance evaluation system test
Abbreviations: ADL: Activities of Daily Living; BBS: Berg Balance Scale; BESTest: Balance Evaluation System Test; HMD: Head Mounted Device; HO: Null Hypothesis; Ha: Alternative Hypothesis; HR QoL-Health Related Quality of Life; MOCA: Montreal Cognitive Assessment; PBBT: Perturbation Based Balance Exercise; SPSS-Statistical Package of Social Sciences; SIS-Stroke Impact Scale; TUG-Timed Up and go Test; VR-Virtual Reality; VR BESS: Virtual Reality Balance Error Scoring System
Effect of Balance Exercises with Smart Phone Based Virtual Reality Programme on Balance in Stroke Patients
Nihitha Siriguppa* and Prem Kumar BN
Post Graduate Student, Kempegowda Institute of Physiotherapy, Rajiv Gandhi University of Health Sciences, India
*Address for Correspondence: Nihitha Siriguppa, Post Graduate Student, Kempegowda Institute of Physiotherapy, Rajiv Gandhi University of Health Sciences, India, Email: [email protected]
Background and objectives: A stroke is a neurological deficit, caused due to vascular changes. Impaired postural control and balance impairments in post-stroke patients are associated with a high risk of falls among stroke patients. The perturbation-based balance training is mainly used in older adults and balance impairment. Virtual reality (VR) as a novel technology is rapidly becoming a popular intervention for improving balance. VR can visualize computer-generated environments with a full field of view through Head-mounted displays (HMD-VR). This study was conducted to assess and investigate the effect of balance exercises with smartphone-based virtual reality programs on balance in stroke patients.
Methods: This was a randomized single-group pre and post-test study design. 30 subjects met the inclusion criteria and were enrolled, assigned, and received intervention. Subjects were given perturbation-based balance exercises and smartphone-based virtual reality along with conventional physiotherapy. The intervention protocol was for 6 days/week for 4 weeks period.
Results: Following 4 weeks of intervention showed improvement in postural control and balance which was assessed using BBS, TUG, VR BESS, BESTest, and SIS 3.0. Paired t-test was used to differentiate the mean significance. The mean pre to post-intervention difference is 12.6 with a p - value < 0.05. TUG score improved from pre to post-intervention difference is 1.443 with a p - value < 0.05. VR BESS score improved from pre to post-intervention difference is 10.266 with a p value < 0.05. The mean BESTest pre to post-intervention difference is 11.467 with a p - value < 0.05. SIS 3.0 score improved from a pre to post-intervention difference is 20.33 with p - value < 0.05. The result of this study showed a highly significant difference in pre and post-treatment.
Conclusion: The study concludes that perturbation-based balance exercises with smartphone-based virtual reality programs are a useful adjunct to improving balance in stroke patients along with conventional physiotherapy.
Stroke is classically characterized as a neurological deficit and also neurological emergency attributed to an acute focal injury of the central nervous system (CNS) by a vascular cause, including cerebral infarction, intracerebral hemorrhage (ICH), and subarachnoid hemorrhage (SAH), and is a major cause of disability and death worldwide [1-3].
WHO definition of stroke (introduced in 1970 and still used) is “rapidly developing clinical signs of focal (or global) disturbance of cerebral function, lasting more than 24 hours or leading to death, with no apparent cause other than that of vascular origin. The recommended standard WHO Stroke definition is “a focal or global neurological impairment of sudden onset, and lasting more than 24 hours or leading to death and of presumed vascular origin” [4].
Clinical features as per vascular territory are as follows: In anterior cerebral artery infarct paresis or weakness of legs more than arm with sparing of hands, urinary incontinence, gait apraxia, and akinetic mutism are seen. In the middle cerebral artery infarct homonymous hemianopia, aphasia (Broca’s and Wernicke’s), inattention, gaze paralysis, and paresis of face-arm-leg are seen. In vertebrobasilar artery infarct if the occipital lobe is involved then symptoms like homonymous hemianopia, cortical blindness, and other cortical visual deficits are seen. If the cerebellum is involved then ataxia, and nystagmus are seen. If the brainstem is involved then cranial nerve palsies with diplopia, vertigo, dysphagia, and dysphonia are seen [5-10].
If a spinal tract is involved hemiparesis and hemisensory loss are seen. In lacunar stroke syndromes (due to occlusion of deep perforating small arteries) symptoms like pure motor hemiparesis, pure sensory stroke, sensorimotor stroke, and ataxic hemiparesis are seen [12-14].
Balance is the capability of maintaining the body’s center of gravity within the base of support. Balance activity is mediated by three systems: biomechanical, neurological, and sensory systems. Motor, sensory, and higher brain cognitive faculties to various degrees, which leads to diminished balance, more postural sway, and asymmetric weight distribution.
The novelty of perturbation training is in the focus on speed of processing and execution of limb movements, as well as rapid restabilization; this differs from ‘traditional’ balance training programs using voluntary movements that allow participants to control speed [15-19].
Virtual reality as a novel technology is rapidly becoming a popular intervention for improving balance and proliferated in the field of neurorehabilitation. Interactive multimedia technologies offer certain advantages over traditional rehabilitation treatments either due to accessibility issues, geography, or treatment availability, providing motivational activities, therapeutic adherence, and treatment compliance. In immersive VR we can visualize the computer-generated environments with a full field of view by Head-mounted displays (HMD-VR) [20-27]. This immersive virtual environment which represents a real environment can be used in balance training in which continuous visual feedback [28,29].
Virtual reality can be described in I3 terms:- INTERACTION + IMMERSION + IMAGINATION [30-53].
Conventional physical therapy based on activities of daily living skills includes active assistive exercises for the lower limb and upper limb, active exercises, functional retraining exercises, stretching, strengthening exercises, weight-bearing exercises, weight shifting exercises, reaching exercises in sitting and standing, and gait training.
Aim of the study
The aim of the study is to investigate the effect of balance exercises with smartphone-based virtual reality programs on balance in stroke patients.
Research gap: There are no gaps in knowledge or understanding of a subject. There is no lack of understanding of the mechanisms behind disease and how technology works.
Hypothesis
Null hypothesis: There may be no significant effects of balance exercises with smartphone-based virtual reality programs on balance in stroke.
Alternate hypothesis: There may be significant effects of balance exercises with smartphone-based virtual reality programs on balance in stroke.
Hence we accept the alternative hypothesis and reject the null hypothesis.
The purpose of the study is to investigate the effect of balance exercises with a smart smartphone-based virtual reality program on balance in stroke patients.
Method of collection of data
Study design: Randomized single-group pre and post-test study design.
Sample size: 30
Sample design: Purposive sampling
Study duration: 12 months
Source of data
- Outpatient department and In-patient department of General Medicine in Kempegowda Institute of Medical Sciences Hospital and Research Centre, Bengaluru.
- Out-patient department of physiotherapy in Kempegowda Institute of Medical Sciences Hospital and Research Centre, Bengaluru.
- Out-patient department and inpatient department of neurology, and neurosurgery in Kempegowda Institute of medical science hospital and research center, Bengaluru.
Sample size estimation
- A sample size of an unknown population
- z value - cumulative normal frequency
z = 1.96
- p - power of confidence
- e - margin of error= 0.05 (type I error)
- here,
- p = 95% i.e., 0.05
- So
= 1.96 ×1.96 ×0.05 ×380
= 72.990
- SSukp = 245.6
- A sample size of known population – SSkp
- Here, N = Total number of patients per month
- = 2.5
- SSkp = 72.990
•
- = 2.417
- = 2.47 which is approximately equal to 2.5
- SSkp which is approximately equal to 5
- Therefore, SSkp = 2.5 for one month
- Here, the study duration is 1 year (12 months) so, Sample size = 12×2.417
- = 29.004 ≈ 30
- Therefore, the total sample size = 30
Selection criteria
Inclusion criteria:
1) Patients with Ischemic stroke are diagnosed with a CT scan.
2) Stroke within 45 days.
3) A score of 26 points or higher on the Montreal Cognitive assessment
4) Both genders are included.
5) Subjects who are willing to participate, who have been explained and signed the written informed consent.
Exclusion criteria:
1) Subjects with Perceptual cognitive deficits like hemi spatial neglect, attention, and memory deficit.
2) Subjects with Spinal and lower extremity deformities
3) Subjects with Terminal illness or medically unstable
Materials used:
1) Smartphone
2) Virtual reality- IRUSU MINI
3) IN CELL (game app)
4) Firm mattress
5) Foam mattress
6) Stopwatch
7) Measuring tape
8) Armrest Chair
9) Cones/markers
The subject included will be explained about the intervention in the language understood by the subject/family members. A signed informed consent will be obtained in the subject/family’s own understandable language Figure 1.
Figure 1: Materials used.
Data analysis
Descriptive and inferential statistical analysis has been carried out in the present study. Results on continuous measurements are presented on Mean ± SD (Min-Max) and results on categorical measurements are presented in Number (%). Significance is assessed at a 5% level of significance.
The following are the assumptions of the data;
1) Dependent variables should be normally distributed,
2) Samples drawn from the population should be random, and Cases of the samples should be independent.
Statistical software
The Statistical software namely SPSS is used for the analysis of the data and Microsoft Word and Excel have been used to generate graphs, tables, etc Table 1.
| Table 1: Data collection. | ||||||||||||
| Sl.No | Age | Gender | Berg Balance Scale (BBS) | Timed up and Go Test (TUG) | Virtual Reality Balance Error Scoring System (VR-BESS) | Balance Evaluation System Test (BESTest) | Stroke Impact Scale (SIS 3.0) | |||||
| Day 1 | Day 4th Week | Day 1 | Day 4th Week | Day 1 | Day 4th Week | Day 1 | Day 4th Week | Day 1 | Day 4th Week | |||
| 1) | 51 | Male | 31 | 48 | 13 | 10.93 | 31 | 20 | 80 | 93 | 30% | 75% |
| 2) | 55 | Male | 26 | 44 | 16.8 | 13 | 29 | 11 | 69 | 84 | 60% | 75% |
| 3) | 43 | Male | 36 | 45 | 12.14 | 17 | 30 | 19 | 75 | 83 | 75% | 80% |
| 4) | 66 | Male | 24 | 40 | 16 | 13 | 32 | 26 | 69 | 77 | 60% | 75% |
| 5) | 50 | Male | 33 | 43 | 17.12 | 13 | 33 | 29 | 64 | 76 | 40% | 65% |
| 6) | 55 | Male | 49 | 54 | 16.12 | 12 | 36 | 26 | 58 | 73 | 50% | 75% |
| 7) | 50 | Female | 36 | 45 | 12.14 | 17 | 30 | 19 | 75 | 83 | 75% | 80% |
| 8) | 66 | MALE | 24 | 40 | 16 | 13 | 32 | 26 | 69 | 77 | 60% | 75% |
| 9) | 67 | MALE | 36 | 45 | 12.14 | 17 | 30 | 19 | 75 | 83 | 75% | 80% |
| 10) | 74 | Female | 36 | 45 | 12.14 | 17 | 30 | 19 | 75 | 83 | 75% | 80% |
| 11) | 55 | MALE | 26 | 44 | 16.8 | 13 | 29 | 11 | 69 | 84 | 60% | 75% |
| 12) | 75 | MALE | 36 | 45 | 12.14 | 17 | 30 | 19 | 75 | 83 | 75% | 80% |
| 13) | 60 | Female | 36 | 45 | 12.14 | 17 | 30 | 19 | 75 | 83 | 75% | 80% |
| 14) | 66 | Male | 24 | 40 | 16 | 13 | 32 | 26 | 69 | 77 | 60% | 75% |
| 15) | 42 | Male | 36 | 45 | 12.14 | 17 | 30 | 19 | 75 | 83 | 75% | 80% |
| 16) | 51 | Male | 31 | 48 | 13 | 10.93 | 31 | 20 | 80 | 93 | 30% | 75% |
| 17) | 55 | Male | 26 | 44 | 16.8 | 13 | 29 | 11 | 69 | 84 | 60% | 75% |
| 18) | 50 | Male | 33 | 43 | 17.12 | 13 | 33 | 29 | 64 | 76 | 40% | 65% |
| 19) | 55 | Male | 49 | 54 | 16.12 | 12 | 36 | 26 | 58 | 73 | 50% | 75% |
| 20) | 51 | Male | 31 | 48 | 13 | 10.93 | 31 | 20 | 80 | 93 | 30% | 75% |
| 21) | 66 | Male | 24 | 40 | 16 | 13 | 32 | 26 | 69 | 77 | 60% | 75% |
| 22) | 50 | Male | 33 | 43 | 17.12 | 13 | 33 | 29 | 64 | 76 | 40% | 65% |
| 23) | 55 | Male | 49 | 54 | 16.12 | 12 | 36 | 26 | 58 | 73 | 50% | 75% |
| 24) | 51 | Male | 31 | 48 | 13 | 10.93 | 31 | 20 | 80 | 93 | 30% | 75% |
| 25) | 55 | Male | 26 | 44 | 16.8 | 13 | 29 | 11 | 69 | 84 | 60% | 75% |
| 26) | 50 | Male | 33 | 43 | 17.12 | 13 | 33 | 29 | 64 | 76 | 40% | 65% |
| 27) | 55 | Male | 49 | 54 | 16.12 | 12 | 36 | 26 | 58 | 73 | 50% | 75% |
| 28) | 51 | Male | 31 | 48 | 13 | 10.93 | 31 | 20 | 80 | 93 | 30% | 75% |
| 29) | 55 | Male | 26 | 44 | 16.8 | 13 | 29 | 11 | 69 | 84 | 60% | 75% |
| 30) | 66 | Male | 24 | 40 | 16 | 13 | 32 | 26 | 69 | 77 | 60% | 75% |
Outcome measures
The Montreal Cognitive Assessment (MoCA) is a tool that can be used to systematically and thoroughly assess cognitive and mental status. It is a 1-page, 30-point test, administrable in ≈10 minutes, which evaluates different domains: visuospatial abilities, executive functions, short-term memory recall, attention, concentration, working memory, language, and orientation to time and space. The total possible score is 30, a score of 26 or above is considered normal.
The Berg balance scale (BBS) was originally designed to quantitatively assess balance. The BBS is a 14-item scale that quantitatively assesses balance and risk for falls. The scale requires 10 to 20 minutes to complete and measures the patient’s ability to maintain balance either statically or while performing various functional movements- for a specified duration of time. The BBS measures both static and dynamic aspects of balance.
The timed up-and-go test (TUG) is an objective clinical measure for assessing functional mobility and balance, and thus the risk of falling. The TUG measures the time taken for an individual to rise from a chair, walk 3 meters, turn walk back, and sit down using regular footwear and a walking aid if required. , subjects are asked to stand up from a standard chair with a height of between 40 cm and 50 cm, walk a 3 m distance at a normal pace, turn, walk back to the chair, and sit down.
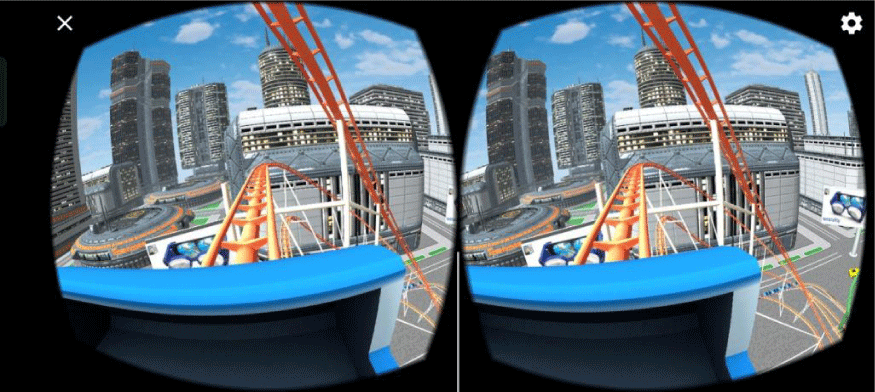
The virtual reality balance error scoring system (VR-BESS) has improved the capability to detect lingering neurological and balance deficits. This involved 3 minutes of sitting followed by 3 minutes of standing while wearing the VR headset and experiencing the rollercoaster stimulus attempting to maintain balance in a two-leg, single-leg, or tandem stance on both foam and firm surface for 20 seconds in each stance Figure 2,3.
Figure 2: VR-BESS: 3-minute VR rollercoaster balance test to detect neurological and balance deficits.
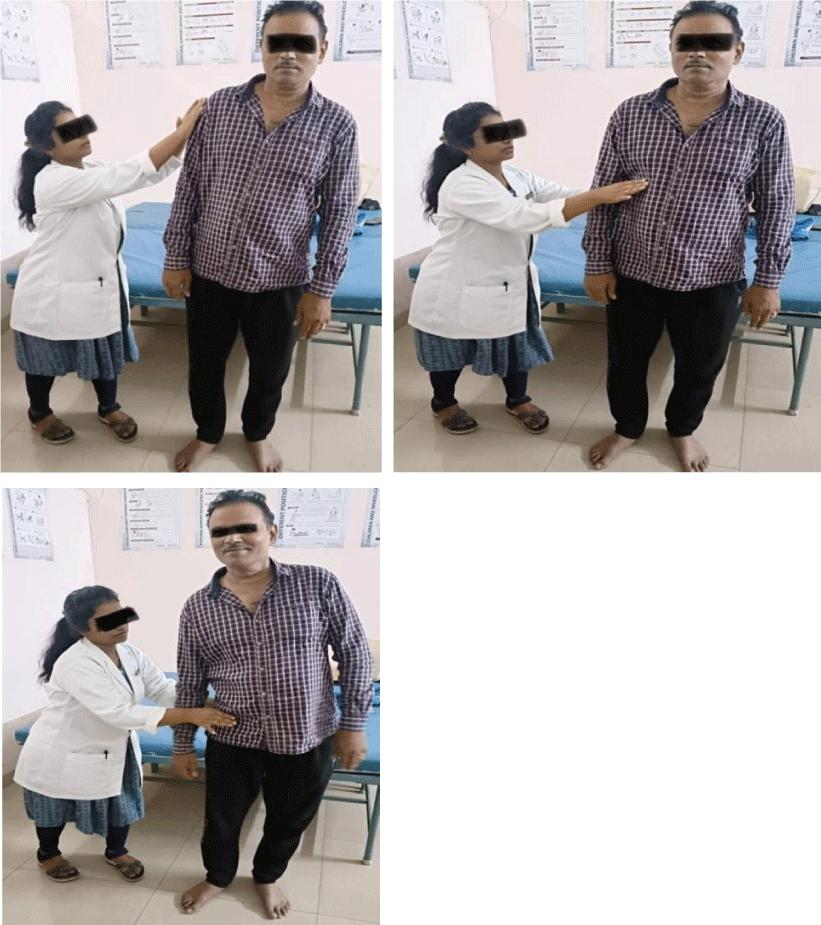
Figure 3: BESTest: Comprehensive balance assessment tool that evaluates different balance systems using 27 tasks and 6 subgroups scored on a 4-level scale.
The Balance Evaluation System Test (BESTest) is a new tool that assesses different balance systems including biomechanical constraints, stability limits/verticality, anticipatory postural adjustments, postural responses, sensory orientation, and gait stability. It is divided into 27 tasks and 6 subgroups, each item is scored on a 4-level, ordinal scale from 0 (worst performance) to 3 (best performance). The total score for the test is 108 points.
The Stroke impact scale (SIS) 3.0 assesses 59 items of a patient’s quality of life, divided into eight dimensions where a stroke has an overall effect on health and well-being. After SIS is administered, the respondent is asked to rate their percent recovery since their stroke on a visual analog scale of 0 to 100 with 0 meaning no recovery & 100 meaning full recovery Figure 4.
Figure 4: SIS 3.0: 59-item stroke impact assessment tool that measures quality of life and recovery.
Intervention
Perturbation-based balance training:
- Perturbations were given in the sitting position on a couch and standing positions, with 10 10-second hold, 10 perturbations in each position, and 5 minutes.
- Perturbations were given in both right and left sideways forward and backward directions in sitting and standing.
- Perturbations were given at the shoulder, trunk and waist region.
Smartphone-based virtual reality training:
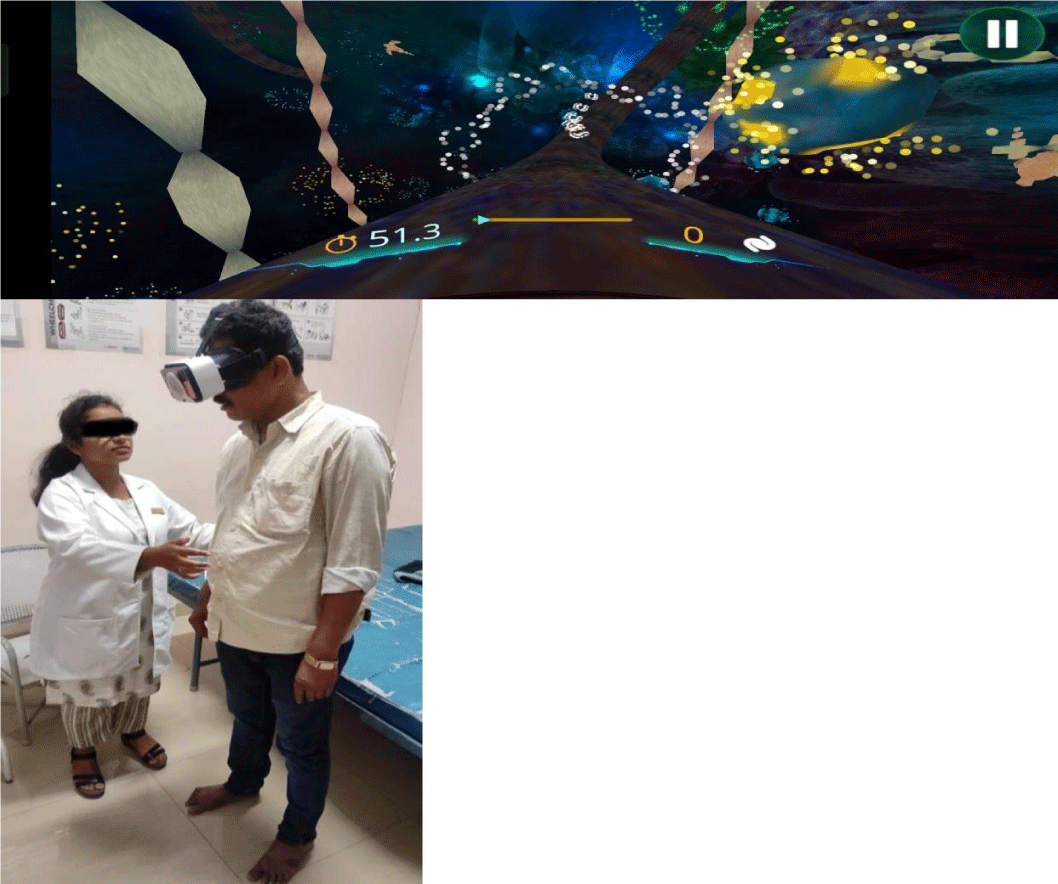
- The therapist explains the neurorehabilitation program based on perturbation-based balance exercise with a head-mounted display virtual reality (IRUSU MINI) with a smart smartphone enclosed in it with the game “IN CEEL VR” and demonstrates the game by showing a screen recording how to play.
- IN CELL VR game is an action racing VR game with a bit of strategy and science thrown into the mix. It will take an exciting journey inside the highly unusual micro world of human cells and stop the virus's advance.
- IN CELL VR game that has specific tasks like hitting the proteins and avoiding the viruses. The subject had to hit the protein and avoid the viruses, which was done in a standing position Figure 5.
Figure 5: IN CELL VR: Virtual reality balance exercise game with protein hitting and virus avoidance tasks.
Interpretations
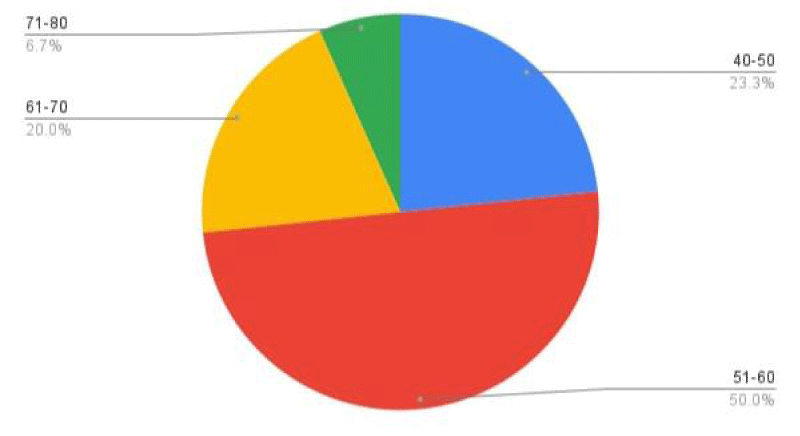
Interpretation: The above Table 2 and Figure 6 show the mean and standard deviation of age. Subjects studied a mean of 56.367 and a standard deviation of 8.29.
| Table 2: Assessment of age. | |
| Missing | 0 |
| Mean | 56.367 |
| Standard deviation | 8.2982 |
| Range | 33.0 |
| Minimum | 42.0 |
| Maximum | 75.0 |
Figure 6: Count of age category..
Interpretation: Using t-statistics and a 5% level of significance. The critical value for the test with df=29 and alpha = 0.05 is 2.045 and the decision rule is to Reject null if the t - value is greater than are equal to 2.045. i.e., calculated value >= critical value Table 3.
| Table 3: An Assessment of Berg balance scale variables at pre and post measurements of patients. | |||
| Variables | Mean | Std. Deviation | |
| BBS | Pre-Score | 32.833 | 7.7819 |
| Post-Score | 45.433 | 4.191 | |
| Difference | 12.6 | 3.5909 | |
| p - value (within the group) - paired t - test | < 0.05** (t = -14.586) | ||
Calculated value = 14.586 and critical value = 2.045.
Hence, we reject null (H0) because 14.586 >= 2.045 and p < 0.05. We have statistically significant evidence at alpha = 0.05 to show there is a difference in the mean of the Berg Balance Scale on day 1 and the day 4th week.
• The result showed a significant difference in Berg balance scale scores within the group (p = 0.00). Hence, we reject the null hypothesis and accept the alternative hypothesis that smartphone-based virtual reality balance training with perturbation-based balance training has a significant effect on stroke.
Interpretation: Using t-statistics and a 5% level of significance. The critical value for the test with degree of freedom and alpha = 0.05 is 2.045 and the decision rule is to Reject null if the t - value is greater than are equal to 2.045. i.e., calculated value >= critical value Table 4.
| Table 4: An Assessment of Timed up and Go Test Variables at pre and post measurements of patients. | |||
| Variables | Mean | Std. Deviation | |
| TUG | Pre-Score | 14.898 | 2.04383 |
| Post-Score | 13.455 | 2.12711 | |
| Difference | 1.443 | 0.08328 | |
| p - value (within the group) - paired t - test | < 0.05** (t = 2.191) | ||
Calculated value = 2.191 and critical value = 2.045.
Hence, we reject null (H0) because 2.191 >= 2.045 and p < 0.05. We have statistically significant evidence at alpha = 0.05 to show there is a difference in the mean of the Timed up and Go test on day 1 and the day 4th week.
• The result showed a significant difference in Timed up-and-go test scores within the group (p = 0.037). Hence, we reject the null hypothesis and accept the alternative hypothesis smart phone-based virtual reality balance training with perturbation-based balance training has a significant effect on stroke.
Interpretation: Using t-statistics and a 5% level of significance. The critical value for the test with degree of freedom and alpha = 0.05 is 2.045 and the decision rule is to Reject null if the t - value is greater than are equal to 2.045. i.e., calculated value >= critical value Table 5.
| Table 5: An Assessment of Virtual Reality Balance Error Scoring System Variables at pre and post measurements of patients | |||
| Variables | Mean | Std. Deviation | |
| VR BESS | Pre-Score | 31.533 | 2.193 |
| Post-Score | 21.267 | 5.9069 | |
| Difference | 10.266 | 3.7139 | |
| p - value (within the group) - paired t - test | < 0.05** (t = 12.867) | ||
Calculated value = 12.867 and critical value = 2.045.
Hence, we reject null (H0) because 12.867 >= 2.045 and p < 0.05. We have statistically significant evidence at alpha = 0.05 to show there is a difference in the mean of the virtual reality balance error scoring system on day 1 and the day 4th week.
• The result showed a significant difference in Virtual reality balance error scoring system scores within the group (p = 0.00). Hence, we reject the null hypothesis and accept the alternative hypothesis that smartphone-based virtual reality balance training with perturbation-based balance training has a significant effect on stroke.
Interpretation: Using t-statistics and a 5% level of significance. The critical value for the test with df=29 and alpha = 0.05 is 2.045 and the decision rule is to Reject null if the t - value is greater than are equal to 2.045. i.e., calculated value >= critical value Table 6.
| Table 6: An Assessment of Balance Evaluation System Test variables at pre and post-measurement of patients. | |||
| Variables | Mean | Std. Deviation | |
| BEST TEST | Pre-Score | 70.1 | 6.9597 |
| Post-Score | 81.567 | 6.4844 | |
| Difference | 11.467 | 0.4753 | |
| p - value (within the group) - paired t - test | < 0.05** (t = -20.604) | ||
Calculated value = 20.604 and critical value = 2.045.
Hence, we reject null (H0) because 20.604>= 2.045 and p < 0.05. We have statistically significant evidence at alpha = 0.05 to show there is a difference in the mean of the Balance Evaluation System test on day 1 and the day 4th week.
• The result showed a significant difference in the Balance evaluation system Test scores within the group (p = 0.00). Hence, we reject the null hypothesis and accept the alternative hypothesis that smartphone-based virtual reality training with perturbation-based balance training has a significant effect on stroke.
Interpretation: Using t-statistics and a 5% level of significance. The critical value for the test with degree of freedom and alpha = 0.05 is 2.045 and the decision rule is to Reject null if the t - value is greater than are equal to 2.045. i.e., calculated value >= critical value Table 7.
| Table 7: An Assessment of Stroke Impact Scale Variables at pre and post measurements of patients | |||
| Variables | Mean | Std. Deviation | |
| SIS | Pre-Score | 54.50% | 15.72% |
| Post-Score | 74.83% | 4.45% | |
| Difference | 20.33 | 11.27 | |
| p - value (within group) - paired t - test | < 0.05** (t = -8.36) | ||
Calculated value = 8.36 and critical value = 2.045.
Hence, we reject null (H0) because 8.36 >= 2.045 and p < 0.05. We have statistically significant evidence at alpha = 0.05 to show there is a difference in the mean of the Stroke impact on day 1 and the day 4th week.
• The result showed a significant difference in SIS scores within the group (p = 0.00). Hence, we reject the null hypothesis and accept the alternative hypothesis that smartphone-based virtual reality balance training with perturbation-based balance training has a significant effect on stroke.
Limitations of the study
1. The sample size was small, limiting the generalizability of the results.
2. The age group was kept wide due to the unavailability of sample size.
3. Only sub-acute stroke patients were included.
4. Study duration was short i.e., only for 4 weeks.
5. The study analyzed only the short-term benefits with respect to mobility, balance, and function.
Future scope and suggestions
1. Future clinical trial studies can be carried out on a large sample size.
2. A similar study can be conducted in patients with different neurological conditions like Parkinson’s, and cerebral palsy.
3. In the present study improvement in balance, and postural control was seen in sub-acute stroke patients, so future studies can also be done to see the effect of perturbation-based balance training on all phases of stroke patients i.e., in acute and chronic.
4. Further studies are needed to investigate the long-term effects of mobile-based virtual reality programs along with conventional physiotherapy treatment balance, and postural control.
Stroke is the leading cause of disability and frequent falling is one of the complications of post stroke. Impaired postural control and balance are associated with a high incidence of falls in stroke. Incidence of fall in stroke, balance exercises is essential.
This study was conducted to find the effect of perturbation-based balance exercises with smartphone-based virtual reality along with conventional physiotherapy. After four weeks of intervention, berg balance scale (BBS), timed up and go test (TUG), virtual reality balance error scoring system (VR BESS), balance evaluation system test (BESTest), stroke impact scale 3.0 (SIS 3.0) were used to analyze the data, results of data analysis showed significant improvement in lower extremity function, balance, gait speed, functional ability, postural stability, muscular coordination, mobility and fall risk.
The findings provide a new paradigm of training guidelines for balance control and can reduce the risk of falling. This perturbation-based balance training with a smartphone-based virtual reality program appears to be feasible and effective for improving balance after ischemic stroke. The findings from our study are clinically important, as they provide an innovative method for the treatment of stroke patients with an efficient, safe, and low-cost program.
- Sacco RL, Kasner SE, Broderick JP, Caplan LR, Connors JJ, Culebras A, Elkind MS, George MG, Hamdan AD, et al. American Heart Association Stroke Council, Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular and Stroke Nursing; Council on Epidemiology and Prevention; Council on Peripheral Vascular Disease; Council on Nutrition, Physical Activity and Metabolism. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013 Jul;44(7):2064-89. doi: 10.1161/STR.0b013e318296aeca. Epub 2013 May 7. Erratum in: Stroke. 2019 Aug;50(8):e239. PMID: 23652265.
- Komlodi-Pasztor E, Gilbert MR, Armstrong TS. Diagnosis and Management of Stroke in Adults with Primary Brain Tumor. Curr Oncol Rep. 2022 Oct;24(10):1251-1259. doi: 10.1007/s11912-022-01280-6. Epub 2022 May 11. PMID: 35543860; PMCID: PMC9474382.
- Coupland AP, Thapar A, Qureshi MI, Jenkins H, Davies AH. The definition of stroke. J R Soc Med. 2017 Jan;110(1):9-12. doi: 10.1177/0141076816680121. Epub 2017 Jan 13. PMID: 28084167; PMCID: PMC5298424.
- Thomas T, Stephen B. The Global Burden of Cerebrovascular Disease. World Health Organization. 2006. https://www.researchgate.net/publication/228551377_The_Global_Burden_of_Cerebrovascular_Disease ( Accessed on April 2022).
- Kamalakannan S, Gudlavalleti ASV, Gudlavalleti VSM, Goenka S, Kuper H. Incidence & prevalence of stroke in India: A systematic review. Indian J Med Res. 2017 Aug;146(2):175-185. doi: 10.4103/ijmr.IJMR_516_15. PMID: 29265018; PMCID: PMC5761027.
- Avan A, Digaleh H, Di Napoli M, Stranges S, Behrouz R, Shojaeianbabaei G, Amiri A, Tabrizi R, Mokhber N, Spence JD, Azarpazhooh MR. Socioeconomic status and stroke incidence, prevalence, mortality, and worldwide burden: an ecological analysis from the Global Burden of Disease Study 2017. BMC Med. 2019 Oct 24;17(1):191. doi: 10.1186/s12916-019-1397-3. PMID: 31647003; PMCID: PMC6813111.
- Kuriakose D, Xiao Z. Pathophysiology and Treatment of Stroke: Present Status and Future Perspectives. Int J Mol Sci. 2020 Oct 15;21(20):7609. doi: 10.3390/ijms21207609. PMID: 33076218; PMCID: PMC7589849.
- Martin S, Kessler M. Neurological Intervention for physical therapy, 4th ed. Evansville, 2021. Chapter 11 stroke pg n. 348-349.
- Smajlović D. Strokes in young adults: epidemiology and prevention. Vasc Health Risk Manag. 2015 Feb 24;11:157-64. doi: 10.2147/VHRM.S53203. PMID: 25750539; PMCID: PMC4348138.
- Patten C, Lexell J, Brown HE. Weakness and strength training in persons with poststroke hemiplegia: rationale, method, and efficacy. J Rehabil Res Dev. 2004 May;41(3A):293-312. doi: 10.1682/jrrd.2004.03.0293. PMID: 15543447.
- Choi HL, Yang K, Han K, Kim B, Chang WH, Kwon S, Jung W, Yoo JE, Jeon HJ, Shin DW. Increased Risk of Developing Depression in Disability after Stroke: A Korean Nationwide Study. Int J Environ Res Public Health. 2023 Jan 2;20(1):842. doi: 10.3390/ijerph20010842. PMID: 36613164; PMCID: PMC9819798.
- PS Prevalence of stroke in k’taka higher than national average Deccan Herald. DH News Service; 2021. https://www.deccanherald.com/state/top-karnataka-stories/prevalence-of-stroke-in-ktaka-higher-than-national-average-1008770.html (Accessed on August 2022).
- Won SH, Kim JC, Oh DW. Effects of a novel walking training program with postural correction and visual feedback on walking function in patients with post-stroke hemiparesis. J Phys Ther Sci. 2015 Aug;27(8):2581-3. doi: 10.1589/jpts.27.2581. Epub 2015 Aug 21. PMID: 26357443; PMCID: PMC4563319.
- Navarro-Orozco D, Sánchez-Manso JC. Neuroanatomy, Middle Cerebral Artery. 2023 Jul 24. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. PMID: 30252258.
- Bernhardt J, Hayward KS, Kwakkel G, Ward NS, Wolf SL, Borschmann K, Krakauer JW, Boyd LA, Carmichael ST, Corbett D, Cramer SC. Agreed definitions and a shared vision for new standards in stroke recovery research: The Stroke Recovery and Rehabilitation Roundtable taskforce. Int J Stroke. 2017 Jul;12(5):444-450. doi: 10.1177/1747493017711816. PMID: 28697708.
- Sheila L, Gita R, Verheyden G. Physical management for neurological conditions Fourth edition Publisher, Elsevier Health Sciences, 2018 ; ISBN, 0702077232, 9780702077234.
- Woodruff TM, Thundyil J, Tang SC, Sobey CG, Taylor SM, Arumugam TV. Pathophysiology, treatment, and animal and cellular models of human ischemic stroke. Mol Neurodegener. 2011 Jan 25;6(1):11. doi: 10.1186/1750-1326-6-11. PMID: 21266064; PMCID: PMC3037909.
- Murphy SJ, Werring DJ. Stroke: causes and clinical features. Medicine (Abingdon). 2020 Sep;48(9):561-566. doi: 10.1016/j.mpmed.2020.06.002. Epub 2020 Aug 6. PMID: 32837228; PMCID: PMC7409792.
- Gund BM, Jagpat PN, Ingale VB, Patil RY. Stroke: A Brain Attack. IOSR Journal of Pharm. 2013; Sept;03(08):01–23.
- Li J, Zhong D, Ye J, He M, Liu X, Zheng H, Jin R, Zhang SL. Rehabilitation for balance impairment in patients after stroke: a protocol of a systematic review and network meta-analysis. BMJ Open. 2019 Jul 19;9(7):e026844. doi: 10.1136/bmjopen-2018-026844. PMID: 31326927; PMCID: PMC6661695.
- Lee K. Speed-Interactive Pedaling Training Using Smartphone Virtual Reality Application for Stroke Patients: Single-Blinded, Randomized Clinical Trial. Brain Sci. 2019 Oct 27;9(11):295. doi: 10.3390/brainsci9110295. PMID: 31717888; PMCID: PMC6895905.
- Liu C, McNitt-Gray JL, Finley JM. Impairments in the mechanical effectiveness of reactive balance control strategies during walking in people post-stroke. Front Neurol. 2022 Oct 31;13:1032417. doi: 10.3389/fneur.2022.1032417. PMID: 36388197; PMCID: PMC9659909.
- Mansfield A, Aqui A, Centen A, Danells CJ, DePaul VG, Knorr S, Schinkel-Ivy A, Brooks D, Inness EL, McIlroy WE, Mochizuki G. Perturbation training to promote safe independent mobility post-stroke: study protocol for a randomized controlled trial. BMC Neurol. 2015 Jun 6;15:87. doi: 10.1186/s12883-015-0347-8. PMID: 26048054; PMCID: PMC4456796.
- Kumar C, Pathan N. Effectiveness of Manual Perturbation Exercises in Improving Balance, Function and Mobility in Stroke Patients: A Randomized Controlled Trial. J Nov Physiother 6: 284. 2016; 6(2): 1-7 doi:10.4172/2165-7025.1000284.
- Inness EL, Mansfield A, Lakhani B, Bayley M, McIlroy WE. Impaired reactive stepping among patients ready for discharge from inpatient stroke rehabilitation. Phys Ther. 2014 Dec;94(12):1755-64. doi: 10.2522/ptj.20130603. Epub 2014 Aug 7. PMID: 25104795; PMCID: PMC4263904.
- Handelzalts S, Kenner-Furman M, Gray G, Soroker N, Shani G, Melzer I. Effects of Perturbation-Based Balance Training in Subacute Persons With Stroke: A Randomized Controlled Trial. Neurorehabil Neural Repair. 2019 Mar;33(3):213-224. doi: 10.1177/1545968319829453. Epub 2019 Feb 15. PMID: 30767613.
- Ooha K, Thulasi P, Apparao P, Prakash P, Ganapathi Swamy C. Effectiveness of mobile based virtual reality training on improving balance in elderly population. European Journal of Pharmaceutical and Medical Research. 2021; 8(12). 369-378.
- Marques-Sule E, Arnal-Gómez A, Buitrago-Jiménez G, Suso-Martí L, Cuenca-Martínez F, Espí-López GV. Effectiveness of Nintendo Wii and Physical Therapy in Functionality, Balance, and Daily Activities in Chronic Stroke Patients. J Am Med Dir Assoc. 2021 May;22(5):1073-1080. doi: 10.1016/j.jamda.2021.01.076. Epub 2021 Feb 24. PMID: 33639116.
- Huygelier H, Schraepen B, van Ee R, Vanden Abeele V, Gillebert CR. Acceptance of immersive head-mounted virtual reality in older adults. Sci Rep. 2019 Mar 14;9(1):4519. doi: 10.1038/s41598-019-41200-6. PMID: 30872760; PMCID: PMC6418153.
- Hao J, Xie H, Harp K, Chen Z, Siu KC. Effects of Virtual Reality Intervention on Neural Plasticity in Stroke Rehabilitation: A Systematic Review. Arch Phys Med Rehabil. 2022 Mar;103(3):523-541. doi: 10.1016/j.apmr.2021.06.024. Epub 2021 Aug 2. PMID: 34352269.
- Li Z, Han XG, Sheng J, Ma SJ. Virtual reality for improving balance in patients after stroke: A systematic review and meta-analysis. Clin Rehabil. 2016 May;30(5):432-40. doi: 10.1177/0269215515593611. Epub 2015 Jul 3. PMID: 26141808.
- Kamińska MS, Miller A, Rotter I, Szylińska A, Grochans E. The effectiveness of virtual reality training in reducing the risk of falls among elderly people. Clin Interv Aging. 2018 Nov 14;13:2329-2338. doi: 10.2147/CIA.S183502. PMID: 30532523; PMCID: PMC6241865.
- Truijen S, Abdullahi A, Bijsterbosch D, van Zoest E, Conijn M, Wang Y, Struyf N, Saeys W. Effect of home-based virtual reality training and telerehabilitation on balance in individuals with Parkinson disease, multiple sclerosis, and stroke: a systematic review and meta-analysis. Neurol Sci. 2022 May;43(5):2995-3006. doi: 10.1007/s10072-021-05855-2. Epub 2022 Feb 17. PMID: 35175439; PMCID: PMC9023738.
- Gutiérrez RO, Galán Del Río F, Cano de la Cuerda R, Alguacil Diego IM, González RA, Page JC. A telerehabilitation program by virtual reality-video games improves balance and postural control in multiple sclerosis patients. NeuroRehabilitation. 2013;33(4):545-54. doi: 10.3233/NRE-130995. PMID: 24029009.
- Pintado-Izquierdo S, Cano-de-la-Cuerda R, Ortiz-Gutiérrez RM. Video Game-Based Therapy on Balance and Gait of Patients with Stroke: A Systematic Review. Applied Sciences. 2020; 10(18):6426. https://doi.org/10.3390/app10186426.
- Shin DC, Song CH. Smartphone-Based Visual Feedback Trunk Control Training Using a Gyroscope and Mirroring Technology for Stroke Patients: Single-blinded, Randomized Clinical Trial of Efficacy and Feasibility. Am J Phys Med Rehabil. 2016 May;95(5):319-29. doi: 10.1097/PHM.0000000000000447. PMID: 26829087.
- Lee MM, Lee KJ, Song CH. Game-Based Virtual Reality Canoe Paddling Training to Improve Postural Balance and Upper Extremity Function: A Preliminary Randomized Controlled Study of 30 Patients with Subacute Stroke. Med Sci Monit. 2018 Apr 27;24:2590-2598. doi: 10.12659/MSM.906451. PMID: 29702630; PMCID: PMC5944399.
- Lin RC, Chiang SL, Heitkemper MM, Weng SM, Lin CF, Yang FC, Lin CH. Effectiveness of Early Rehabilitation Combined With Virtual Reality Training on Muscle Strength, Mood State, and Functional Status in Patients With Acute Stroke: A Randomized Controlled Trial. Worldviews Evid Based Nurs. 2020 Apr;17(2):158-167. doi: 10.1111/wvn.12429. Epub 2020 Mar 25. PMID: 32212254.
- Iqbal M, Arsh A, Hammad SM, Haq IU, Darain H. Comparison of dual task specific training and conventional physical therapy in ambulation of hemiplegic stroke patients: A randomized controlled trial. J Pak Med Assoc. 2020 Jan;70(1):7-10. doi: 10.47391/JPMA.10443. PMID: 31954014.
- Suda S, Muraga K, Ishiwata A, Nishimura T, Aoki J, Kanamaru T, Suzuki K, Sakamoto Y, Katano T, Nagai K, Hatake S, Satoi S, Matsumoto N, Nito C, Nishiyama Y, Mishina M, Kimura K. Early Cognitive Assessment Following Acute Stroke: Feasibility and Comparison between Mini-Mental State Examination and Montreal Cognitive Assessment. J Stroke Cerebrovasc Dis. 2020 Apr;29(4):104688. doi: 10.1016/j.jstrokecerebrovasdis.2020.104688. Epub 2020 Feb 14. PMID: 32063455.
- Dautzenberg G, Lijmer J, Beekman A. Clinical value of the Montreal Cognitive Assessment (MoCA) in patients suspected of cognitive impairment in old age psychiatry. Using the MoCA for triaging to a memory clinic. Cogn Neuropsychiatry. 2021 Jan;26(1):1-17. doi: 10.1080/13546805.2020.1850434. Epub 2020 Dec 3. PMID: 33272076.
- Blum L, Korner-Bitensky N. Usefulness of the Berg Balance Scale in stroke rehabilitation: a systematic review. Phys Ther. 2008 May;88(5):559-66. doi: 10.2522/ptj.20070205. Epub 2008 Feb 21. PMID: 18292215.
- Miranda-Cantellops N, Tiu TK. Berg Balance Testing. 2023 Feb 17. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. PMID: 34662032.
- Hafsteinsdóttir TB, Rensink M, Schuurmans M. Clinimetric properties of the Timed Up and Go Test for patients with stroke: a systematic review. Top Stroke Rehabil. 2014 May-Jun;21(3):197-210. doi: 10.1310/tsr2103-197. PMID: 24985387.
- Rausch M, Simon JE, Starkey C, Grooms DR. Smartphone virtual reality to increase clinical balance assessment responsiveness. Phys Ther Sport. 2018 Jul;32:207-211. doi: 10.1016/j.ptsp.2018.05.017. Epub 2018 May 22. PMID: 29803943.
- Chinsongkram B, Chaikeeree N, Saengsirisuwan V, Horak FB, Boonsinsukh R. Responsiveness of the Balance Evaluation Systems Test (BESTest) in People With Subacute Stroke. Phys Ther. 2016 Oct;96(10):1638-1647. doi: 10.2522/ptj.20150621. Epub 2016 Apr 21. PMID: 27103226; PMCID: PMC6281077.
- Sahin IE, Guclu-Gunduz A, Yazici G, Ozkul C, Volkan-Yazici M, Nazliel B, Tekindal MA. The sensitivity and specificity of the balance evaluation systems test-BESTest in determining risk of fall in stroke patients. NeuroRehabilitation. 2019;44(1):67-77. doi: 10.3233/NRE-182558. PMID: 30814369.
- Almalki O, Alshehri MA, El-Fiky AA, Abdelaal AA, Alzaidi JH, Al Attar WSA, Hegazy FA. Can the stroke impact scale 3.0 detect cognitive impairments in patients with a recent stroke? J Phys Ther Sci. 2019 Jul;31(7):563-568. doi: 10.1589/jpts.31.563. Epub 2019 Jul 9. PMID: 31417222; PMCID: PMC6642892.
- Vellone E, Savini S, Fida R, Dickson VV, Melkus GD, Carod-Artal FJ, Rocco G, Alvaro R. Psychometric evaluation of the Stroke Impact Scale 3.0. J Cardiovasc Nurs. 2015 May-Jun;30(3):229-41. doi: 10.1097/JCN.0000000000000145. PMID: 24695074.
- Prakash V, Ganesan M, Vasanthan R, Hariohm K. Do Commonly Used Functional Outcome Measures Capture Activities that Are Relevant for People with Stroke in India? Top Stroke Rehabil. 2017 Apr;24(3):200-205. doi: 10.1080/10749357.2016.1234190. Epub 2016 Sep 27. PMID: 27671020.
- Cheng YS, Chien A, Lai DM, Lee YY, Cheng CH, Wang SF, Chang YJ, Wang JL, Hsu WL. Perturbation-Based Balance Training in Postoperative Individuals With Degenerative Cervical Myelopathy. Front Bioeng Biotechnol. 2020 Feb 20;8:108. doi: 10.3389/fbioe.2020.00108. PMID: 32154235; PMCID: PMC7044125.
- Iruthayarajah J, McIntyre A, Cotoi A, Macaluso S, Teasell R. The use of virtual reality for balance among individuals with chronic stroke: a systematic review and meta-analysis. Top Stroke Rehabil. 2017 Jan;24(1):68-79. doi: 10.1080/10749357.2016.1192361. Epub 2016 Jun 16. PMID: 27309680.
- Fritz SL, Peters DM, Merlo AM, Donley J. Active video-gaming effects on balance and mobility in individuals with chronic stroke: a randomized controlled trial. Top Stroke Rehabil. 2013 May-Jun;20(3):218-25. doi: 10.1310/tsr2003-218. PMID: 23841969.