More Information
Submitted: September 26, 2023 | Approved: November 08, 2023 | Published: November 09, 2023
How to cite this article: Gupta VK. Bimatoprost Ophthalmic Solution (BOS) 0.3 mg w/v for 1 Open Trial of Long-term Preventive Therapy of Migraine in 3 patients with Pathophysiologic Shift from Brain to Eye. J Neurosci Neurol Disord. 2023; 7: 134-154.
DOI: 10.29328/journal.jnnd.1001087
Copyright License: © 2023 Gupta VK, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Migraine; Psychosocial stress; ANS-dysfunction; Choroido-retinal arterial circulation; Intraocular pressure; Ocular globe; Corneoscleral envelope; Corneoscleral distention; Pan-trigeminal; Ophthalmic division of trigeminal nerve (V1); Mechanical pronociceptive neural traffic; Ocular rigidity; Tamponade; Elasticity; Spontaneous onset; Spontaneous offset; Ebstein anomaly; Congenital heart disease; Morbid obesity; Female preponderance; Age-linked prevalence
Bimatoprost Ophthalmic Solution (BOS) 0.3 mg w/v for 1 Open Trial of Long-term Preventive Therapy of Migraine in 3 patients with Pathophysiologic Shift from Brain to Eye
Vinod Kumar Gupta*
Physician-Medical Director, Gupta Medical Centre, Migraine-Headache Institute, S-407, Greater Kailash, Part Two, New Delhi-110048, India
*Address for Correspondence: Dr. Vinod Kumar Gupta, MB, BS, MD (Internal Medicine), Physician-Medical Director, Gupta Medical Centre, Migraine-Headache Institute, S-407, Greater Kailash, Part Two, New Delhi-110048, India, Email: [email protected]
Known since antiquity, migraine is a complex primary disorder, an episodic painful Autonomic Nervous System (ANS) storm, generally following the stress/post-stress phase. Despite exhaustive study of neuropeptides, neurochemicals, molecules, neurogenetics, neuroimaging along with animal and human experiments over the last 50 years, the scientific basis of migraine remains unknown. Straddling eight decades from Cortical Spreading Depression (CSD) to Calcitonin-Gene Related Peptide (CGRP) and its antagonists, exponentially increasing data have failed to create a gestalt synthesis. This article lays cohesive and robust fundamental principles for the comprehension and management of migraine. The continuum between migraine and non-congestive Primary Open-Angle Glaucoma (POAG), Normal Tension Glaucoma (NTG), or Low-Tension Glaucoma (LTG) is advancing. The case of sustained remission of migraine attacks (> 75%) over 3 years - 5 years with ocular hypotensive topical Bimatoprost Ophthalmic Solution (BOS) 0.3% in an N-of-1 trial in 3 patients with refractory migraine is presented. A cause-effect-adaptive process underlies the ANS-stress/post-stress-linked biology of migraine. Vasopressin-serotonin-norepinephrine ‘homeostatic-adaptive system’ Lowers Intraocular Pressure (IOP), while enhancing anti-stress, antinociception, vasomotor, and behaviour control functions, thereby selectively decreasing algogenic neural traffic in the ophthalmic division of trigeminal nerve (V1), and, raising the threshold to develop migraine. Striking migraine headache-aborting feature of vomiting is also likely linked to a several hundred-fold increase in arginine-vasopressin secretion. Eye-cover tests and self-ocular digital displacement are essential to studying the visual aura. Real-time physical displacement of Scintillating Scotoma (SS) and floating ‘stars’ is reported. The basis of spontaneous onset and offset, self-limited duration of migraine attacks, as well as female preponderance, and age/menopause decline in prevalence, are elucidated. Intraocular implants with long-term ocular hypotensive effects, including bimatoprost, are the future of migraine management. Controlled trials are required to establish the migraine-preventive effect of topical bimatoprost, a revolutionary advance in neuroscience.
AH: Aqueous Humor; AMT: Amitriptyline; AN: Anxiety Neurosis; AVP: Arginine Vasopressin; BBB: Blood-Brain Barrier; CM: Chronic Migraine; CSD: Cortical Spreading Depression; NTG: Normal Tension Glaucoma; EA: Ebstein Anomaly; EM: Episodic Migraine; NTG: Nitroglycerine; LTG: Low-Tension Glaucoma; MwA: Migraine with Aura; MwoA: Migraine Without Aura; MO: Morbid Obesity; OAG: Open-Angle Glaucoma; ONH: Optic Nerve Head; POAG: Primary Open-Angle Glaucoma; RCCT: Randomized Controlled Clinical Trials; RNFL: Retinal Nerve Fibre Layer; m-GCIPL: Macular Ganglion Cell Inner Plexiform Layer; m-RNFL: Macular Retinal Nerve Fibre Layer; p-RNFL: paramacular Retinal Nerve Fibre Layer; RSD: Retinal Spreading Depression; SBP: Systemic Blood Pressure; SD: Spreading Depression; SD-OCT: Spectral Domain Optical Coherence Tomography; V1: Ophthalmic Division of the Trigeminal Nerve; VM: Valsalva Maneuver
Migraine is a common poorly understood typically-protean primary painful disorder characterized by episodic, moderate-to-severe, often pulsating, and more frequently-than-not lateralizing headache (unilateral, bilateral, side-shifting, or side-fixed) associated with photophobia, phonophobia, nausea/vomiting, and sometimes auras (visual or non-visual or both [1-4]. Consistently ranked as one of the most disabling neurological conditions affecting ~20% of the general population, migraines often substantially impairs daily activities (personal, family, social, and professional) as well as quality of life and carries a high economic burden of direct and indirect healthcare costs (emergency care, abortive and preventive therapies, and absenteeism or presenteeism) [1,5,6]. Migraine is currently regarded as a social stigma [7-9]. Migraine has been split into Episodic Migraine (EM) and Chronic Migraine (CM) by the criterion of 15 headache days in a month [10,11]. Such nosologic splitting of migraine is based entirely on symptomatic phenotypic expansion, and is a commonsense-challenging subdivision resulting in exponential accumulation of data without any pathophysiologic insight or matrix/blueprint [11]. Neuronal dysmodulation, central neural plasticity and sensitization are believed to underlie the progression from EM to CM [10-14]. Cross-species circumstantial or indirect evidence, largely from animal experiments (mainly, rodents) with direct extrapolation to humans, form the speculative basis of the currently-favored belief-stimulated pathogenesis of both subtypes of migraine -- EM and CM [11,15,16].
Etiology of migraine, both EM and CM subtypes, however, continues to be elusive and its mechanistic basis remains speculative, with multiple discrete and rather diverse physiologic disease mechanisms being proposed and supported over the last 2 decades – usually as per the presumed basis of a few common phenotypic symptoms [1,17-20]. All key elements of migraine have never been incorporated into a single biologically-plausible, robust, generalizable, and overarching gestalt synthesis [11]. Fundamental pathophysiologic difference(s) between Migraine with Aura (MwA) and migraine without aura (MwoA) are also maintained through speculative interpretation of the basis of phenotype, underscoring a prominent dichotomy running between migraine pathophysiology and migraine neuro-pharmacology. No clinically substantial or statistically significant and replicable difference between MwA and MwoA subtypes has been found in their responses to pharmacotherapeutic or non-pharmacotherapeutic strategies. First- and second-line migraine preventive pharmacotherapeutic drugs show comparable efficacy in MwA patients and MwoA patients, thereby not supporting the widely-supported ‘two entity’ research presumption. An extraordinary amount of scientific effort and literature has been devoted to creating, maintaining, and studying the two ‘imaginary’ nosologic subdivisions of migraine, both EM and CM as well as MwA and MwoA. Not surprisingly, statistically significant therapeutic differences between these nosologic subdivisions have been underscored [1-3,10,14,18-29]. These therapeutic assertions of any statistical difference between subdivisions of migraine (EM v/s CM; MwA v/s MwoA) are not clinically valuable or practically useful, and the scientific foundation of the supporting data itself not being are theoretically-robust [11,15,16,30-34] All therapies in migraine are empirical, including those supported by Randomized Controlled Clinical Trials (RCCTs) [15,16,30,31,35,36], By a canonical but belief-based general consensus among primary headache researchers over the last fifty years, migraine is currently believed to originate in a vague dysfunction of the brain that lends no insight into spontaneous onset and offset of protean, periodic onset (cyclic menstrual or non-cyclic non-menstrual), and self-limited duration (4 hours - 72 hours) of headache. Similarly, the scintillating Scotoma (SS) of MwA appears and disappears spontaneously in an equally bizarre and mysterious manner, the time period being foreshortened to 30-60 minutes. The Blood-Brain Barrier (BBB) is not disrupted during migraine attacks [37,38]. Many researchers favour a meningitic basis as the source of migraine headaches; the nature of the meningitic process and its ability to produce unpredictable lateralizing self-limited headaches for decades or a lifetime raises reservations. To the best of my knowledge, the role of the presumed ‘meningitic’ process in the genesis of SS of migraine finds no mention in the literature. Neuronal, vascular, and neurovascular theories have variably prevailed over the last 50 years without any definitive headway [11,15,16] [Gupta 2006]. The chicken-egg controversy has never been solved in migraine: how does cranially-lateralizing headache or SS just appear de-novo, and then spontaneously disappear or resolve by itself?
Seven decades after the chance discovery of Cortical Spreading Depression (CSD) in rodents, key issues remain unsettled. [11,15,16,39] Spreading Depression (SD) has been recently recorded during multimodal neuromonitoring in neurocritical care and is believed to represent a universal principle of cortical lesion development from asphyxia/anoxia to traumatic brain injury; not unexpectedly. therapeutic suppression of SD has been suggested [40,41] There is no link between the pain of migraine headache – the most bothersome symptom – and CSD/SD, as reviewed [11,15,16,35].
Conversely, CSD has well-defined adaptive/homeostatic neuronal protective and vascular preconditioning role in lower mammals, locusts, and Drosophila [Box 1].
| Box 1: Adaptive / Homeostatic Effects of Cortical Spreading Depression / Spreading Depression in brain neuronal and vascular function. |
|
|
|
|
|
|
|
|
|
|
|
| Other favoured pathophysiological hyopotheses from over a100 years previously will be discussed later in this article under discussion in an organized manner with absolute principles/laws. |
Migraine, as a co-morbidity, confounds contemporary clinical glaucoma evaluation and management. Migraine has been reported more commonly in Primary Open-Angle Glaucoma (POAG); after adjusting patients’ age and vascular comorbidities, migraineurs were found to have a 1.68 - fold (95% confidence interval, 1.20 - 2.36) greater risk of developing OAG than the comparison cohort [70]. The migraine-POAG link was found in case-control design studies but not in cohort design studies [71]. Association was also noted between migraine and Low-Tension Glaucoma (LTG) [72,73]. Across studies of the migraine-glaucoma continuum, without assessment of visual function dysfunction, a clinically subtle heterogeneity confounds the association, both with POAG and Primary Angle-Closure Glaucoma (PACC), particularly with cross-sectional population-based studies or retrospective analyses of insurance-related databases [74,75]. In an epidemiologic survey with key diagnostic glaucomatous features established by ophthalmologists, including IOP, glaucomatous optic disc cupping, nerve bundle visual field defect, open anterior chamber angles, atrophy of ONH, and no discernible cause of outflow obstruction, migraine prevalence did not significantly differ between high IOP-glaucoma (IOP > 21 mm Hg) and LTG (IOP < 21 mm Hg) patients (22.8% and 32%, respectively) [72].
Migraine attacks are associated with a wide range of visual sensory symptoms [76,77]. In prospective studies, visual performance tests allow a clearer clinical correlation between glaucoma and migraine than cross-sectional epidemiologic or retrospective studies. Growing evidence suggests inter-ictal visual function impairment in migraine with standard tests of visual function necessary for the diagnosis and monitoring of glaucoma (visual fields, electrophysiology, ocular imaging). These abnormalities are measurable in between migraine events, despite patients being asymptomatic and otherwise healthy [78]. Habituation of Visually Evoked Potentials (VEP) also significantly differ in subgroups in the migraine cohort, influenced by the presence or absence of perceived stress or family history of migraine or hyperventilation or disease heterogeneity as markers of arousal [79-81]. Interictal habituation studies do not report uniform results [82]. Ocular (scleral/choroidal/retinal) activation, functional or structural, will invariably also affect the brain’s cortical and subcortical regions, and visual impairment in migraine is apparently of retinal origin, a distinction made over three decades previously [83,84].
Structural changes in the papillary retina and ONH are shared between migraine and glaucoma. Reduction of mean peripapillary retinal nerve fibre layer thickness (pRNFL), mean macular ganglion cell-inner plexiform layer (mGCIPL) and macular retinal nerve fibre layer (mRNFL) detected with spectral domain optical coherence tomography (SD-OCT) is a sensitive feature of diagnostic value in glaucoma; statistically significant sectoral thinning of inferior and temporal functional subzones best differentiate changes between controls and glaucoma patients [85,86] Similarly, in migraineurs, meta-analysis with large datasets strengthens the clinical evidence of RNFL thinning via SD-OCT as well as significantly larger optic disc rim area and foveal avascular zone optical coherence tomography angiography [87-89].
Mean choroidal thickness and subfoveal choroidal thickness are also significantly thinner in migraine, both in MwA and MwoA patients than healthy controls, as well as both in-between attacks (inter-ictal phase) and during headache attacks (ictal phase) [90-94]. Non- homonymous visual field loss is reported during headache attacks in migraine patients, decreasing but persisting as long as 75 days in a cohort of MwoA patients [76,95-97]. In asymptomatic interictal periods, visual surround suppression for drifting stimuli is greater in migraine patients than in controls [98]. This behaviourally measurable imbalance in inhibitory and excitatory visual processes in migraine is not compatible with a simple model of reduced cortical inhibitory function within the visual system.
The amount of CGRP-monoclonal antibodies (CGRP-mAbs) that enter the brain, if at all, is too small to be even physiologically meaningful; certainly, there is no evidence to suggest that a critical pharmacotherapeutic modulation of central brain neuronal function underlies the migraine preventive action of these agents [6,11,32,99-102]. Decreased activation of hypothalamic nuclei or spinal tract of trigeminal nerve or both by monoclonal antibodies to CGPR in human migraine patients [103] does not exclude effects of secondary modulation of cranial sensory traffic by CGRP from outside the brain neurovascular system [11,15,16].
The largest number of known migraine-modulating clinical, experimental, and pharmacological factors – both increasing susceptibility or decreasing susceptibility to induce migraine attacks – are linked to the ocular choroid-IOP-corneoscleral system [11,15,16,30,31,38,81,84,104,105].
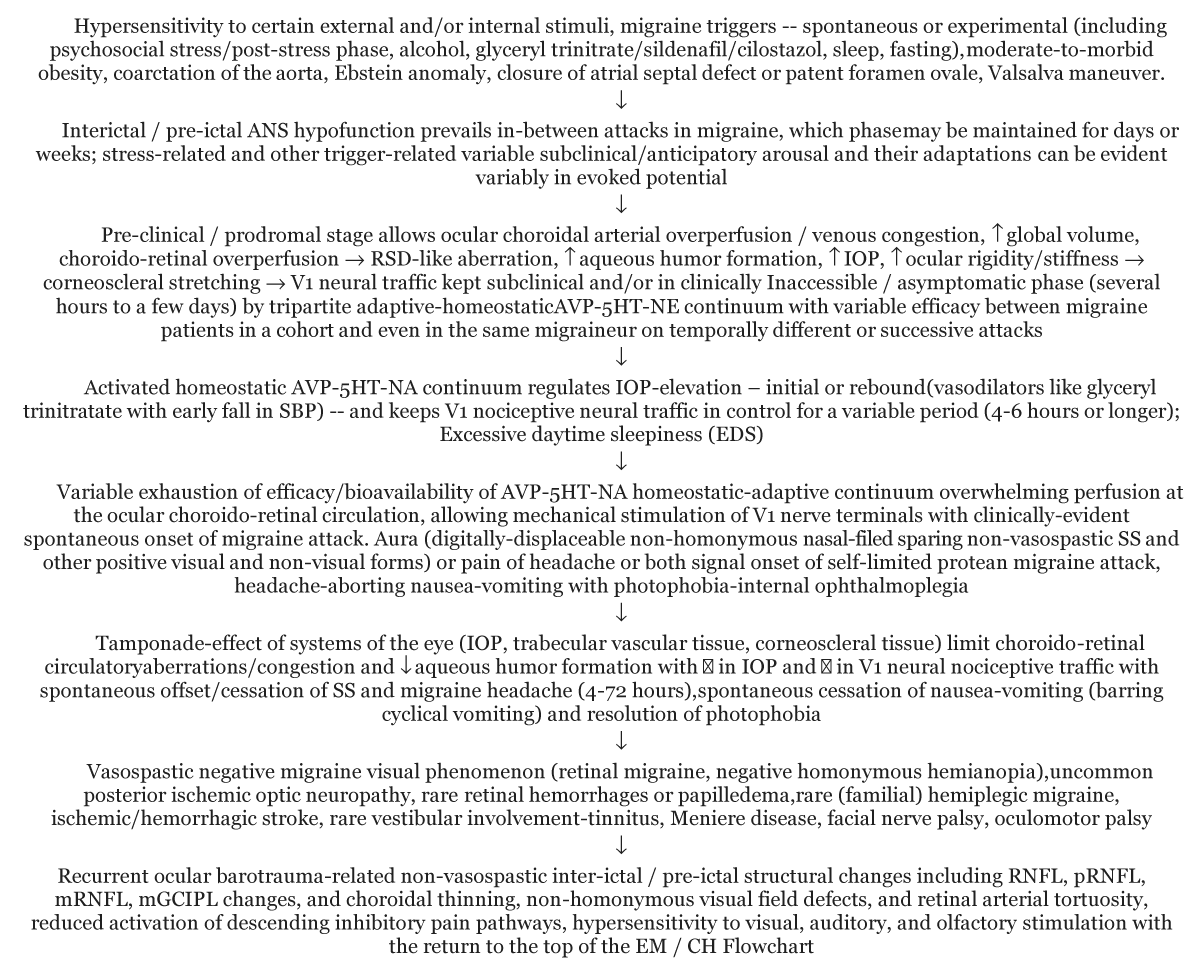
In placebo-controlled Randomized Clinical Trials (RCCTs) to abort migraine attacks, ocular hypotensive therapy with timolol maleate ophthalmic solution has not been found consistently useful [106-110] In a double-blind placebo-controlled crossover trial, propranolol in oral doses up to 120 mg/day was ineffective in controlling acute attacks of migraine aura or headache or both [111]. The failure of propranolol (40 mg) to abort migraine headache was also observed in a previous study [112]. Conversely, positive results with propranolol in the therapy of acute migraine attacks were reported earlier [113,114]. The ocular pathophysiology of the acute headache phase of migraine with self-cycling and self-limited choroido-retinal congestion and algogenic V1 nerve traffic is completely different from that of the pre-headache / pre-clinical phase of migraine without choroido-retinal congestion and algogenic neural traffic in V1, as discussed below [Figure 1].
Figure 1: Flow-chart of proposed Rapid Time-Frame Linked Pathogenetic Algorithm for recurrent spontaneous EM and CM. Legend: AVP-5HT-NA: Arginine Vasopressin-Serotonin-Noradrenaline; IOP; Intraocular Pressure; RNFL: Retinal Nerve Fibre Layer; mRNFL: macular; mGCIPL: Macular Ganglion Cell-Inner Plexiform Layer; pRNFL: peripapillary Retinal Nerve Fibre Layer; SS: Scintillating Scotoma; V1: Ophthalmic Division of Trigeminal Nerve; EDS-EM: Episodic Migraine; CM: Chronic Migrain.
In a previous study, nocturnal topical (eye instillation) of a single drop of timolol maleate long-acting ophthalmic preparation (0.5% w/v) before going to sleep once-weekly (pre-weekend, Saturday night) in the eye ipsilateral to the weekend-migraine headache in 2 patients were shown to prevent migraines consistently over an extended period of time (≥ 3 years) [30]. Clinical evidence is now presented for the first time for a sustained (3 years - 5 years) migraine attack-preventive role for Bimatoprost Ophthalmic Solution (BOS) 0.3% in 10 patients with refractory migraine attacks. The biologically defensible mechanistic continuum between migraine, ANS hypofunction, choroidal circulation, IOP, and glaucoma is further advanced in this article.
BOS is an established prostaglandin analogue for reducing elevated IOP by promoting AH outflow in patients with POAG and OH. In the absence of existing ethical guidelines, the Food and Drug Administration of the United States of America (FDA, U.S.A.) has a long-standing ethical policy to permit the trial of an already established pharmacotherapeutic agent for a new clinical indication – a policy consistent with reason and logic (see later).
The key systems focus in this article is on the absolute and exclusive role of the eye in spontaneous genesis (onset) and cessation (offset) of the non-homonymous nasal visual field- sparing SS (15 minutes - 60 minutes (and other less well-defined forms of positive visual aura) as well as self-limited lateralizing headache (4 hours - 72 hours) through predominantly stress / post-stress and ANS hypofunction-primed ocular choroidoretinal congestion-linked corneoscleral envelope distention with the generation of self-limited V1 orthodromic and antidromic algogenic neural impulses in migraine. Three principles or laws of migraine pathophysiology have been evolved; these laws robustly rationalize the entire phenomenology of migraine, and, are discussed in this article.
Case report of N-of-1 pilot study with BOS 0.3%
Therapeutic use of topical BOS 0.3 mg/ml for prevention of migraine attacks in 10 migraine patients (8 with Episodic Migraine [EM] and 2 with Chronic Migraine [CM]) were studied between 2015 - 2020. Ethical use of a therapeutic agent already in the market, such as bimatoprost, for a new and unconnected or unconnected indication is permitted to advance science by the FDA, U.S.A.
Diagnosis of migraine (episodic or chronic) was made according to the criteria of the International Classification of Headache Disorders-3 [4]. Inclusion criteria for this study were as follows: (i) migraine headache recurrences and suffering for over 10 years (> or = 100 episodic attacks or > or = 300 headache days), with or without aura symptoms; (ii) 8-weeks basal observation after the first consultation; (iii) migraine headache severity at least 5/10 on a Visual Analog Scale (VAS), with at least 4 attacks or > 30 days of headache in the basal period of 8-weeks basal observation; (iv) exposure to 4 (or more) different migraine preventive drugs under the care of other hospital-based physician/neurologist/ophthalmologist/psychiatrist/pain specialist/headache specialist/ physiotherapist, with each regimen having been followed for at least 4 weeks; (iv) graduate education; and (v) willingness to maintain a Smartphone-based daily record of headache, lateralization of headache, occurrence of nausea/vomiting, fatigue, insomnia, side effects of therapy, or any other associated symptom(s) for ≥ 8-weeks after first consultation. For every migraine headache attack/day, the severity of pain in the first 24 hours as well as duration were to be noted. Exclusion criteria were explicit: Patients with dry eyes, eye discharge, eye pain, allergic conjunctivitis, periorbital or eyelid edema, foreign body sensation in the eye, epiphora, visual blurring, or photophobia in the inter-ictal period, using dark shades indoors or blue-light suppressing glasses, depression, insomnia, moderate-to-severe hypertension, diabetes type 1 or 2, biochemical evidence of hematologic or liver, renal or thyroid disorders, alcohol (mis)use, pregnancy, complex medical history requiring the use of corticosteroids or other immunosuppressives or NSAIDs, or naïve or unable to understand the need for extended preventive management strategy over years/decades did not take part in the study.
Psychosocial stress aggravation (graded from + to ++++) and straining at stools with eyes/open or closed position were required to be noted on a daily basis. No patient with thunderclap headache or ‘worst possible’ headache was included. Neck pain in 1 patient was regarded as bilateral migraine.
Potential for increased brown pigmentation of the iris, for hair growth on skin contact, was advised, and running of BOS 0.3% onto the cheek was strictly prohibited. The occurrence of asymptomatic conjunctival hyperemia for a few hours following BOS instillation was recommended to be ignored.
Written informed consent was obtained on the lines of the ethical principles published by the World Medical Association, adopted as the Declaration of Helsinki, 1964, with later modifications. Current peer comprehension of migraine pathophysiology and all available medical/surgical/interventional therapies were discussed at length without any hesitation or bar with all selected patients, with participants allowed to raise questions and issues through Google Search / Google Scholar. Given the unknown pathophysiology of migraine, the protection of the human participants in this study as well as their long-term overall interests was kept primary at all levels. Withdrawal from the study was always presented as an option. The theoretical basis for this study has evolved over 3 decades and published extensively. Interpretation of all ethical principles involved in this study was not prescriptive. The most important components of the study were the definitive explanation of self-limited visual events and self-limited headaches associated with migraines with spontaneous onset and offset for both key phenomena.
As part of the methodology, the eye-cover test and digital finger displacement tests to evaluate the source of retinal positive-negative crescents or other visual phenomena that have never been explained properly to any migraine patient cohort. Photographs of SS and its breakdown or other variants available from texts in medical periodicals were shown and explained to the 10 participants in this study. The nasal and visual halves of the visual field of each eye were explained to the participants in detail. Monocular and binocular visualization of visual objects was clarified. Personal experience of displacement of the physiologic positive-negative retinal scintillating crescents/arcs following gentle digital-finger self-compression of eyes (right and left, alternatively) with their own index finger was taught to patients to let them know what was critically expected of them.
From the 9th week onwards, patients were instructed to instil 1 drop of BOS 0.3 mg/ml in the eye(s) corresponding to the dominant side of headache, unilaterally or bilaterally, before going to sleep once daily. Patients were also instructed to keep their eye/eyes closed for at least 2 minutes after the instillation of BOS 0.3% and to maintain light pressure on the inner canthus of one or both eyes to diminish the amount of drug reaching systemic circulation, and to remove excess solution with absorbent tissue. Self-instillation of BOS was encouraged; otherwise, assisted instillation from another person was also permitted. The use of analgesics/triptans to manage the pain of migraine headaches was not discontinued. Use of opiate-like tramadol as an analgesic was not permitted.
Headache was bilateral in 3 patients, predominantly right-sided in 5 patients, and left-sided in 2 patients. The age range was 14 years - 62 years, with 7 females and 3 males. Menstrual migraine was reported by 2 females. For the purpose of analysis, headache-pain severity of VAS ≥ 5/10 only was considered. 2 patients reported habitual daily straining at stools. General physical examination of migraine patients was unremarkable. An ophthalmoscopic examination was performed for optic disc and macular retinal evaluation. 7 of 10 patients (70%) reported ≥ 75% reduction in frequency of migraine attacks/days with over 3 years - 5 years. 3 of these 7 patients (42.9%) required 2 instillations of BOS 0.3% (12 hours apart, daily). In the remaining 3 of 10 patients (30%), with ≥ 60% control of migraine attacks/days, high-level anxiety (grade +++/+++++was noted and confirmed with Spielberger’s State-Trait Anxiety Inventory (SSTAI) against the most highly correlated 3 anxiety-present items -- tension, upset, and worried and the most highly correlated 3 anxiety-absent items – calm, relaxed, and content [115]. These 3 patients with moderate-to-severe Anxiety Neurosis (AN) could not by themselves instil BOS 0.3%. Care-takers instilling BOS 0.3% in these 3 anxious migraine patients reported a particularly exaggerated apprehension to the instillation with resistive eye closure required to be overcome forcefully. Of these 2 migraine patients with photophobia-unrelated fear-induced blepharospasm, one patient with pronounced AN (++++) revealed a new clinical phenomenon of anticipatory fear-related repetitive high-frequency tremor-or flutter-like blepharoclonus just before the instillation of BOS 0.3%. The resistance to opening her eyes while supine, her fearful inability to look up to permit conjunctival sac(s) instillation of BOS 0.3%, and the high-frequency non-photophobic blepharoclonus were reconfirmed.
Exacerbation of domestic / workplace psychosocial stress or the post-stress phase was the major trigger for migraine attacks in 8/10 (80%) patients in this study; 6 (60%) patients reported insomnia, and 4 (40%) reported alcohol imbibition, particularly on weekends. 4 patients noted eyes-open straining-at-stools as a migraine trigger, with 2 patients immediately developing ‘stars’ (~50 in number) floating away (to disappear) into the superior temporal edge of the visual field in the right eye followed almost simultaneously with right-sided migraine headache (severity 5/10 on VAS). A single female patient, age 35 years, reported a well-developed non-homonymous nasal-field sparing SS in the temporal visual field of the right eye minutes during 10-15 minutes of 5 migraine attacks. All 3 patients with migraine-related visual phenomena, performed an eye-cover test to find that the rippled SS (1 patient) and the floating ‘stars’ (2 patients) were confined to the right eye (monocular), corresponding to the side of the headache. The SS as well as the floating ‘stars’ were found to be digitally displaceable by gentle self-finger pressure. During straining-at-stools, 4 migraine patients (40%) (3 males and 1 female) noted a tendency to keep both eyes open. Enlarged cupping of the optic disc was detected in 1 migraine patient. Retinal arterial tortuosity in the form ‘v’ or ‘u’ patterns was seen in 3 migraine patients.
Hypersensitivity to BOS 0.3% (bimatoprost or excipients) or increased pigmentation of periorbital tissue (eyelids), eyelashes, and iris were neither reported nor noticed 6 of 10 (50%) patients reported conjunctival hyperemia; the hyperemia lasted 10 hours - 12 hours and was seen only in the palpebral conjunctiva, with the bulbar conjunctiva being spared. Although BOS-induced conjunctival hyperemia is the most frequent treatment-related adverse effect in up to one-third of patients, as per the manufacturer, the restriction of hyperemia to the palpebral aperture has never been previously reported and helps to differentiate from the red-eye of inflammatory/infective conjunctivitis. No other local or systemic side-effect listed by the manufacturer (Allergan, Waco, Texas, 76712, U.S.A.) was reported in this study.
This is the first clinical report of a prospective pharmacologically specific and biologically-defensive sustained N-of-1 study of the preventive effect of topical BOS 0.3%, Aqueous Humor (AH) outflow-promoting IOP-lowering prostaglandin analogue, in 10 patients with long-standing (> 10 years) uncomplicated migraine, either Episodic Migraine (EM) or Chronic Migraine (CM). The preventive ocular hypotensive therapeutic effect of BOS 0.3% was observed consistently in this study in migraine for 3 years - 5 years with ≥ 75% reduction in headache attacks (EM) as well as in headache days (CM), and this is the preliminary report of an ongoing study started in 2015. Every month, all participants in the study were given the option of withdrawing from the study. To date, no patients have withdrawn from the study. In a previous N-of-1 study, the preventive role of long- acting timolol maleate ophthalmic solution 0.5% w/v administered once weekly on Saturday night in the headache-ipsilateral eye, to prevent migraine attack following oversleeping the next morning, i.e., Sunday morning was demonstrated in weekend migraine without any systemic beta-blockade cardiovascular influence for the first time in primary headache literature [30]. Immediate migraine headache-aborting influence of self-applied ocular tamponade has been also reported in another long-term ongoing study [31].
Intriguingly, due to the nature of its neuroanatomy, including high choroido-retinal vascularity as well as the self-limiting tamponade effect of ocular hydrodynamics/haemodynamics, the eye is the only ANS-stress-linked organ in the head-and-neck region that can periodically or cyclically generate: (i) self-limited non-homonymous SS (15 minutes - 60 minutes) likely due to choroido-retinal overperfusion / congestion and mechanical stimulation; and (ii) self-limited (4 hours - 72 hours) lateralizing headache linked to choroidal over-perfusion, the rise of IOP, and ocular anterior segment related-congestion induced corneoscleral distention-stretch-related algogenic neural traffic in V1 distribution [11,15,16,30,31,38]. While stress / post-stress phasic ANS-hypofunction in conjunction with high choroidal vascularity can transiently generate a relatively high IOP in migraine patients, the naturally-available tamponade-limiting force of IOP itself on ocular choroidal blood vessels (higher than elsewhere in the body) combined with the relative elasto-rigidity of corneoscleral tissues that, in turn, contribute to ocular tissue properties offering a second source of tamponade that limits both the rise of IOP as well as corneoscleral distensibility-related nociceptive neural impulses in V1 with self-limitation of the duration of headache or migraine. The tamponade effect of the eye, overall, affects IOP, ocular choroidal vascularity, and corneoscleral distensibility [105,116-118] This change in mechanical stretch-related V1 nociceptive traffic-generating IOP is relative and transient and might be evident only with direct continuous non-invasive recording of IOP with pressure-measuring contact lens sensors (with the capacity to measure the concentration of other tear-fluid-based parameters such glucose, urea, proteins, nitrite, chloride ions, corneal temperature, pH, as well as biomechanical stiffening of the corneoscleral or trabecular meshwork, peripapillary scleral structural changes, and optic nerve head remodelling [119-122].
Migraine (and other primary headaches), ultimately, relate to ocular rigidity linked to self-limited biomechanical changes in retinal (ocular blood-flow-related) and corneoscleral (V1 nociceptive neural traffic) ocular tissues with a spontaneous tamponade effect derived from components of ocular rigidity [11,15,16,30,31,38]. The self-limiting nature of IOP- elevation as part of dynamic and very rapid autoregulation of ocular blood flow-choroidal circulatory- corneoscleral elasto-rigidity nexus in the face of cranio-ocular ANS hypofunction is the single most important physiological event contributing to the highly characteristic self-limited aura- and non-aura (SS or headache or both) phenomenology or phenotype of migraine and other primary headaches.
The link between migraine, ANS dysfunction/hypofunction, IOP, and glaucoma continues to evolve. A very large number of migraine-modulating influences, including critical links with stress/post-stress phase, that can trigger or remit attacks are known to be linked to the increase or decrease in IOP, respectively, a full discussion of which is beyond the scope of this article [11,15,16,30,31,38,104,105,123]. Key migraine modulating psychosocial stress/post-stress and cranio-ocular physiologic changes include: (i) bioavailability / efficacy of the adaptive/ homeostatic arginine vasopressin-serotonin-noradrenalin nexus; (ii) cardiac output; (iii) common carotid/external carotid arterial perfusion; (iv) cranio-ocular ANS hypofunction; (v) ocular choroido-retinal arterial overperfusion; (vi) cranio-ocular choroidal venous congestion, particularly in congenital heart disease including Ebstein anomaly and moderate-to-morbid obesity; (vi) hydrostatic increase in AH secretion with a flow-related rise in IOP; (vii) increase in global volume/distention; (viii) rheological or mechanical segmental-sectoral nasal-sparing temporal retinal spreading depression (RSD) or RSD-like activation of retinal tissue leading to self-limited SS and/or other positive-negative scotoma; and, (ix) mechanical corneoscleral distention leading to V1 algogenic neural traffic (orthodromic or antidromic or both) generating lateralizing headaches. [Figure 1, see text below] First-and second-line migraine preventive pharmacologic agents some of which are established by RCCT such as the prototypic beta-blockers (propranolol, atenolol, or nadolol) and amitriptyline, melatonin, flunarizine, (Angiotensin-Converting Enzyme-Inhibitors (ACE-Is), Angiotensin Receptor Blockers (ARBs) and others clearly lower IOP – a pathophysiologic and pharmacologic absolute [11,15,16,30,31,38,83,84,104,105] The tissue components of corneoscleral distensibility are part of an elaborate connective tissue disorder wherein genetic (trait) factors will complement the state (acquired factors). The placebo factor will also confound clinical/investigative pathophysiologic issues and interpretations. A fuller discussion of these ocular elasto-rigidity factors as well as pharmacologic effects with relevance to migraine pathophysiology is beyond the scope of this article.
Thinning of pRNFL, mGCIPL, mRNFL, and mean and subfoveal choroidal layers recorded via SD-OCT in the inter-ictal headache-free and headache periods, similar to changes in glaucoma also indicate a definitive primary involvement of the posterior pole of the eye [70-75,77,78,85-91,93,95,97] A vasoconstrictive influence on the posterior pole of the eye, as commonly presumed, is highly unlikely to prevail in-between migraine attacks (inter-icital periods). An ‘occult’ relative barometric influence coupled with outlier-enhanced corneoscleral distensibility / ocular rigidity is the most likely cause for prolonged alterations of RNFL and choroidal thickness found in migraine, up to 75 days after an attack.
Canonical pathognomonic SS as well as typical headaches of migraine are not experienced after enucleation of the eye(s) or loss of sight [124-130] Absence of relative or absolute elevation of IOP in migraine [Devisogullari, et al. 2014] [131,], is the missing evidentiary link. Nevertheless, with the onset of exposure to the trigger or anxiety/post-anxiety phase or onset of headache pain early in the course of the migraine attack, the vasopressin-serotonin-noradrenaline homeostatic nexus is activated. Once pain-of-headache is triggered, a relatively low IOP would be maintained. As discussed above, in migraine patients, stress- and other migraine trigger-related homeostatic activation of Arginine-Vasopressin (AVP) raises SBP but lowers the IOP – a most characteristic feature maintains antinociception and behavior control to a protean / variable exhaustible point-in-time that varies between migraine patients in any cohort as well as in the same patient on different temporal occasions. [11,15,16,38,83,84,132] This is the true meaning of ‘protean’ insofar as migraine is concerned, and is invaluable pathophysiologically.
Phase-by-phase phenotypic descriptions and phasic underpinning(s) of discrete pathophysiologic modes for each phase, as is common in migraine literature [1,20,133], is a form of contradictory and artificial individuality or ‘reductionalism’ – as are nosologic ‘hypersplitting’ and/or disparate or stand-alone laboratory ‘evidence’ – operating sans an overarching matrix through a biologically implausible and -an unimaginative mix of speculative but reflexive systemic and /or brain vascular and neuronal theories supporting ‘central’ and/or ‘peripheral’ sensitization.
Critical limitations of CSD as the key pathogenetic have been discussed and found obsolete. The adaptive or homeostatic role of CSD in the animal kingdom is clear in lower mammals and insects. [see Box 1, above] Several key migraine preventive or provocative pharmacologic agents do not influence CSD [11,15,16,30,31,38,84,132]. Glyceryl Trinitrate (GTN), the best-defined i.v. experimental model for migraine headache has no basic or critical influence on basic parameters of KCL-induced CSD, with only a decrease in propagation failure compared to controls [134]. The unexplained but characteristic delay (4 hours - 6 hours) between i.v. administration of GNT and onset of migraine-like headache may be linked to early fall in SBP/IOP or concomitant activation of the homeostatic-adaptive AVP-5HT-NA nexus or both. Cilostazol and sildenafil are other vasodilators, that experimentally produce migraine headaches, importantly most without migraine aura, and none with well-formed SS [135-138] Sildenafil alters neither CSD nor the subsequent characteristic effect of nitric oxide synthase (NOS) inhibition, i.e. a marked widening of CSD [139] Sildenafil raises IOP but lowers SBP [140]. In a small highly-selective cohort of 16 MwA patients, of whom 11 patients (69%, > 2/3rd) only experienced MwA sans headache, sildenafil induced aura symptoms -- but not SS. No migraine headache attack generating experimental systemic vasodilator, including GTN or sildenafil or cilostazol or Calcitonin-Gene Related Peptide (CGRP) has induced SS or other major positive aura-linked symptoms of migraine, barring rare anecdotes, thus sustaining the major pathophysiologic disconnect between the aura and the headache of migraine. Despite widespread belief, experimental vasodilator-induced migraine attacks post-NTG infusion is associated with delayed (1.5 hours - 5.5 hours), diffuse, mild, and transient vasodilatation (6.7% - 30.3%, p < 0.01), while during migraine attacks blood vessel diameters of cerebral or meningeal arteries were no different from baseline or between headache and non-headache sides [141-143] Major arteries such as internal carotid arteries and basilar arteries showed no change in blood flow during NTG-infusion or migraine [143]. Inconsistent vasodilation of the middle meningeal artery followed systemic diffuse vasodilator-induced generalized vascular dilatation not lateralizing to the side of headache [136,138].
Failure of significant dilatation of cerebral arteries (≥ 50% - 75%) following vasodilator challenge indicates the operation of an early rapidly adaptive-homeostatic, spontaneous, and sustained vasoconstrictor influence involving a vasopressin-like neurohormone; such failure of key cranial arteries to vasodilate following NTG-challenge also cannot rationalize lateralizing headache or non-homonymous nasal visual-field SS and/or visual field defects of migraine [11,15,16,83,84,132] Intriguingly, alcohol – one of the commonest precipitants of migraine attacks worldwide – does not dilate but constricts the internal carotid circulation – a feature that has never been underscored in migraine pathophysiology. Ethanol blood concentrations during binge drinking [18 to 80 mM] constrict cerebral arteries in a wide variety of species, including humans, both ex vivo and in vivo; as reviewed, this cerebral vasoconstrictive action of ethanol results from drug-induced inhibition of cerebrovascular smooth muscular K+ vasodilator channels (calcium-and voltage-gated potassium channels of large conductance type) [144,145].
High prevalence of migraine in moderate-to-morbid (total-body and abdominal) obesity, with striking prevalence in Congenital Heart Disease (CHD) without right-to-left shunting (43%), and even higher in Ebstein anomaly (EA) (67%) appears to be directly and sequentially linked to the right ventricular dysfunction and/or obstructive impediment of cranial venous return, cranio-ocular-ANS hypofunction-mediated ocular choroidal arteriovenous congestion and retinal venodilatation, the rise of hydrostatic pressure, IOP elevation, ocular globe, and corneoscleral distention, with the genesis of algogenic V1 neural traffic that is self-limited by the ocular tamponade effect (see algorithm, Figure 1) [146-159].
Closure of Atrial Septal Defect (ASD) can generate migraine de novo or aggravate pre-existent migraine that is likely consequent to immediate or almost-immediate improvement in left-ventricular filling and the concomitant rise in both cardiac output and ocular blood flow (Gupta 2006) [160] Rise of ocular blood flow coupled to ANS-hypofunction in migraine patients can lead to ocular choroidal overperfusion, the rise of ocular hydrostatic pressure, and increased formation of AH with a relatively higher IOP. Patients who undergo device-closure of ASD have much shorter recovery than those who require surgery and thus enjoy the benefits of improved hemodynamics and increased systemic cardiac output much earlier. Neuropathologically, there is no conceivable pathogenetic link of EA, other CHD, obesity, or ASD-closure or PFO-closure to CSD [15,16,161]. Migraine attacks speculatively linked to PFO-related right-to- left atrial shunt with systemic transfer of migraine-attack-provoking substances such as neurotransmitters, further suppose episodic/periodic (cyclical or non-cyclical) elevation of right- atrial pressure through VM, similarly cannot logically rationalize the occurrence of recurrent periodic (programmed, regularly appearing, or cyclic menstrual migraine attacks) or non-periodic (irregularly irregular non-cyclic migraine attacks) self-limited (4 hours - 72 hours) and protean (varied frequency, severity, and duration lateralizing headache predominantly confined to V1 or non- homonymous nasal-visual field sparing SS, that appear spontaneously at puberty, adolescence, adulthood, the first trimester of pregnancy, and spontaneously resolve with later trimesters of pregnancy or advancing age, including menopause [11,159,162]. Size of PFO consistently, but paradoxically, increases with age, while migraine prevalence falls with increasing age, including menopause, as reviewed elsewhere [161]. Results of placebo-controlled trials of PFO closure to prevent migraine attacks and the meta-analyses that follow are not uniform or striking, with the fundamental supporting basis of science lacking and with the primary end- points not being met [161-167] (see below).
Botulinum toxin – type A (BOTOX-A) has no anti-nociceptive or vasomotor-control or behaviour-control role in the management of pain per se or that of em [168,169]. Chronic migraine management with onabotulinum toxin-A is largely disappointing, as in RCCT, migraine frequency is marginally reduced only by 2 days/month [170-172]. Botulinum therapy for the prevention of a long-term disorder such as migraine is also not cost-effective. Magnesium is a vasodilator and does not freely cross the BBB under many discrete experimental circumstances, key issues that render its exogenous administration or supplementation useless for migraine prevention [11]. The role of magnesium as a prophylactic for migraine, as a brain neuronal saviour, and as a life-saving drug in the ICU has become obsolete almost 3 decades previously [173].
Outcome
This study reports in real-time and real-world outside of RCCTs the first N-of-1 evidence for the instantaneous and definitive physical displacement of migraine visual aura, including SS and floating ‘stars’, by the simple measure of guarded and gentle digital self-application of mechanical pressure to both eyeballs alternatively at the inner and outer canthi, thereby establishing beyond doubt that the retina is the source of origin of migraine-related positive visual aura. Monocular non-homonymous distribution of SS confined to the temporal visual field in a migraine patient trained to study her own visual phenomenon is reported for the first time in migraine literature. Such pre-trial training to study participants or volunteers for clinical self-evaluation and self-reporting of visual aura has never been previously made available to migraine patients. Hupp, Kline, and Corbett, in their landmark, ground-breaking, and insightful article three decades ago, suggested that digital / finger displacement of visual phenomena by migraine patients themselves would offer conclusive evidence for retinal or cortical origin of visual aura, uncluttered with statistics; these authors also recommended that migraine patients be trained themselves perform the eye-cover test to determine monocular or binocular distribution of visual aura/phenomena, positive or negative, as well as to distinguish nasal and temporal visual fields of each eye [77].
Migraine attacks can develop unilaterally or bilaterally, and non-homonymous SS or other positive visual aura also may occur in one or both eyes. Bilateral non-homonymous rippled SS-like or floating ‘star-like’ visual aura can mimic homonymously distributed phenomena and misleadingly suggest brain cortical visual cortex origin, unless checked bilaterally / binocularly for digital / finger displacement. Hence, the digital displacement of positive visual phenomena reported in this study accurately determines its retinal origin, regardless of the underlying retinal-level pathophysiologic mechanism(s). Retinal Spreading Depression (RSD) is a well-established neuro-ophthalmologic phenomenon, that can well explain the spreading nature of SS of migraine [174-176]. CGRP receptors mediate RSD propagation while sumatriptan blocks SD in isolated chick retina; RSD is an efficient in vitro approach for assessing anti-migraine drugs targeting CGRP receptors [177,178]. As suggested 2 decades ago, RSD is the only CNS electrical phenomenon that can be activated by mechanical or rheologic pressure (Gupta 2006).
Regardless of underlying cellular/molecular level retinal mechanism(s), [179] absolute clinical evidence regarding displaceable short-lasting neurophysiologic oculo-retinal symptomatic phenomena can be further established with simple but specific training imparted to lay migraine patients without professional knowledge of visual pathway neuroanatomy. Clinical awareness and application of the twin tests of eye cover and self-displacement to determine the side of occurrence and site of origin of visual aura phenomena must be disseminated and improved. Neurologists and headache specialists have the highest incidence of migraine attacks; female headache specialists have 1-year and lifetime migraine prevalence of 74.1% and 81.5% [180,181]. Once the simple but almost-completely ignored neuro-ophthalmologic principle is generally accepted, digital-finger self-displacement of positive migraine aura can be easily replicated and can rapidly establish the precise bio-neural substrate of migraine attacks, including nasal-visual field sparing SS, lateralizing migraine-headache, and painless photophobia versus light-sensitivity. There is no evidence to suggest that the Trigeminovascular ‘System’ (TVS) directly innervates the neurons of the visual cortex to generate a nasal-visual field sparing SS of migraine [11,182]. Also, it is not known why the visual aura should be the preponderant cerebral component of the aura of migraine. Definitive evidence regarding displaceable nasal-visual field sparing SS/positive visual aura can easily come from neurologists, ophthalmologists, headache specialists, and physicians once the exclusive pathophysiologic turf-like hyperfocus on the brain is resolved.
Unspecific brainstem, hypothalamus, and cortex-related activations or evidence will only then be clarified as secondary phenomenological features of migraine [84,183,]. In maintaining brain neuronal hyper-excitability as the pathogenetic basis of migraine [182], the combined brain neuronal-serotonergic and -noradrenergic activation effected by migraine preventive agents (such as AMT) or drugs of abuse (such as cocaine) is an important caveat [11,15,16,184,185] Caffeine is another brain neuronal noradrenergic stimulant – besides AMT or cocaine -- that delays the onset of migraine / migraine-like headache [30]. Neurotransmitters, like CGRP, in general, work in vivo in a very rapid counter-balancing well-orchestrated manner and never in isolation [6,32,99]. Neuro-biological substrate of migraine will become apparent and can be defended robustly against scientific and logical challenges only after the division of its vast phenomenology into primary and secondary components (Gupta 2009). Neurotransmitters or neuropeptides do not constitute the biology of migraine; they simply work as messengers of brain neurons, always in an adaptive-homeostatic mode or concert, never alone. Migraine researchers have divided the whole into parts, all the while, paradoxically, expecting the gestalt to emerge.
This study also reports abnormal retinal arterial tortuosity in migraine for the first time in the scientific literature, first detailed in the Rolex Awards for Enterprise, 1990 [84]. Increased ictal retinal arterial blood flow due to ophthalmic artery overperfusion and ophthlamic venous congestion in migraine may underlie retinal / pre-retinal hemorrhages, papilledema, and glaucomatous optic disc enlargement that have been noted previously in migraine, as part of idiopathic ischemic optic neuropathy [77,186-189]. Such changes are not ischemic but result from over-perfusion. Such choroido-retinal overperfusion, with or without moderate-to-morbid obesity, CHD without right-to-left shunting, EA, or right heart congestion can also be associated with subtle retinal arterial tortuosity consequent to rheological hemodynamic forces. (see above) Retinal arterial tortuosity and venular dilatation are common in CHD, including EA with tricuspid regurgitation / right heart dysfunction, arrhythmia, progressive central cyanosis from right-to-left atrial level shunting, paroxysmal atrial tachyarrhythmias with or without atrioventricular bypass tracts, conjunctival hyperemia, cyanotic fundus hue, papilledema, and rarely visual snow syndrome [146]. Apparently, CHD, including EA and moderate-to-morbid obesity have no pathogenetic link with CSD/SD or any other brain neuronal network or neurovascular dysfunction. On the other hand, obesity is an independent risk factor for elevated IOP in adults as well as in school children, with higher IOP correlated with body mass index (BMI), waist circumference, and diastolic blood pressure (DBP) (see above). Obesity increases adipose tissue in eye sockets, episcleral venous pressure, and corticosteroid secretion while decreasing aqueous outflow due to excessive blood viscosity, which features an increased IOP. Additionally, obesity is also related to diseases that affect OH, hypertension, diabetes, and dyslipidemia. In individuals with Morbid Obesity (MO), respiratory muscles are inefficient and have low performance. Morbid obesity affects the cardiopulmonary system resulting in lower tidal volume, decreased functional residual capacity, higher respiratory rate, lower lung and chest compliance, higher elastic and muscle work, lower strength and endurance of respiratory muscles, higher oxygen consumption and higher levels of fatigue, shallow breathing post-anesthesia, and subclinical hemodynamic dysfunction with impaired venous return from lower limbs and abdomen notably in gynecoid obesity followed by cardiac decompensation with enhanced preload and afterload and severe physical deconditioning [159,190]. In MO, a prominent upwards displacement or ‘splinting’ of the diaphragm by a massive increase in abdominal contents and intra-abdominal pressure is likely another major component of positive intrathoracic pressure, besides visco-elastic splinting of the lung/chest wall musculature. Upward displacement/splinting of the diaphragm in MO constitutes, in effect, a near-constant or -persistent VM-like congestive influence on cranio-ocular circulation, rather than a transient effort- or Valsalva Maneuver (VM)-related intermittent pathophysiologic influence. Cranio-ocular congestion is intrinsic to right ventricular dysfunction from any cause, including EA and MO. The 5 - cm canonical indicator of elevated jugular venous pressure is also probably not relevant to MO; a 2 - cm elevation of (Jugular Venous Pressure) JVP is clinically more representative in MO [191]. Valsalva maneuver is relevant to migraine phenomenology, as an IOP-elevating attack-provoking trigger and or headache-worsening factor, as well as to headache- aborting effortful/forceful nausea/vomiting that itself raises IOP but also intensely stimulates AVP release from posterior neurohypophysis [132,161,192,193]. Strikingly, VM involves ocular venous congestion or backpressure but does not directly or primarily affect the ophthalmo-retinal arterial circulation.
A new pelvic-ocular ANS reflex relevant to VM-related straining-at-stools and VM-related migraine is described. The eyes tend to maintain an open position during pelvic straining during passing stools or flatus or during the pelvic delivery of the foetus, possibly as a conserved or evolutionary ‘guarding’ reflex against social embarrassment and ‘fear’ of uncontrolled pelvic damage or tear. Nevertheless, maintenance of this pelvic-ocular reflex largely transmits VM-related raised intrabdominal/intrathoracic pressures directly, repeatedly, and dramatically to the eyes, particularly with breath-holding [194-196] with ocular globe expansion, venous congestion, raised hydrostatic pressure, increased formation of AH, and rise of IOP. Previously, it has been recommended that the eyes be firmly closed as well as the mouth be kept open to short-circuit the ocular hemodynamic effects of VM to prevent primary headache induced by cough (benign cough-induced headache), to prevent migraine attacks, and to prevent reversible cerebral vasoconstriction syndrome-related thunderclap headache during repetitive and most forceful VM known to humans during labour or pelvic delivery [31,197-199]. Blinking of eyes or forceful closure of eyes (‘screwing’ or ‘squeezing’ eyes shut tightly) can raise IOP to 10 mmHg or as high as 90 mmHg, respectively [200]. The Tamponade effect of raised IOP / elasto-rigidity of ocular tissue structures does not permit uncontrolled choroido-retinal arteriovenous congestion or triggering of certain headache variants, e.g. migraine and cluster headache do not co-exist commonly, indicating major differences in ocular tissue elasto-rigidity.
- Female preponderance;
- Age-related decline in prevalence; and,
- Biological or dynamic-functional rapidly-developing physiologic processes surrounding the stress / post-stress / depression / or other triggers that precipitate the disorder by generating self-limited nasal-visual field sparing SS and lateralizing self-limited headache (4 hours - 72 hours).
From serotonin (1960s) to the CGRP/CGRP-A in the present era (3rd decade of the 21st Century), a series of biochemical and neuroimaging laboratory events or ‘bio-markers’ have displaced the biology of migraine [11]. Statistics-based RCCTs allow – and continue to allow -- migraine researchers to perform legitimate science and to mine migraine-related data without clinical validity or commonsense displacing the abstract qualitative from the quantitative [11,161]. RCCTs, paradoxically, in a cart-before-the-horse manner determine the science of migraine, rather than the other way about. The colossal harm done by mathematical statistics to science and scientific thinking, in general, has only recently aroused the scientific community without a personal or philosophical commitment to any or all disciplines, including the science of migraine / primary headaches [201,202]. While decades of journal columns overemphasizing opinions, evidence from animal experiments with almost direct extrapolation to human migraine patients, RCTs, genetics, and epidemiology have been devoted to possible or presumed canonical but mythologic etiologies/pathophysiologies, such as meningeal activation, neuroinflammation, neuropeptide or molecular releases such as cytokines, oxidants-antioxidants, brain neuronal networks and their activations, white-matter hyperintensities, besides SD and CSD, the genuine chicken-egg scientific questions are never formulated. Why should CSD or molecular-substance releases occur in the first instance in a self-limited manner? Nature abhors a vacuum, and science abhors lack of generalization. What is not generalizable in science/medicine is not true. A full detail of all molecular substances implicated in migraine cannot be absorbed in this article.
The meaning of the term ‘biology’ or ‘biological’ has been lost in migraine research. The ‘biology’ of any illness…is a holistic, gestalt, comprehension… that is not synonymous with ‘nonenvironmental’, ‘organic’, ‘ laboratory’ or even ‘physiological’,…or a ‘unifactorial’ (PFO- or botulinum toxin- or CGRP-like) or a ‘hopelessly complex obfuscation’ or frustrating self-defeating Gordian knots in series and in parallel that constitute a grand ‘nihilism’, but a meticulously orchestrated concatenation of several physiological processes (primary versus secondary stress adaptive/protective/homeostatic physiologic processes) that push or pull the patient towards the disease (migraine-attack or ictal state) or disease-free state (migraine-attack free inter-ictal phase).
Four fundamental physico-biological laws of migraine complete the science of the disorder
- Migraine is a lateralizing cranial painful disorder -- a ‘megrim/hemicranial’ headache that is unilateral, bilateral, side-shifting, or side-fixed. From serotonin to SBP to CRGP/CGRP-A, no systemic influence can rationalize the pathophysiology of migraine [173].
- Migraine is a selective algogenic ophthalmologic nerve (V1) disorder, not a pan-trigeminal disorder. Neck pain in migraine attacks is part of V1 innervation [11].
- Migraine is frequently aborted by nausea-vomiting, a powerful stimulus for AVP-release from the neurohypophysis with vasomotor, antinociceptive, and behaviour control mechanisms [132].
- SS (unilateral or bilateral) of migraine spares the nasal-visual field and is physically displaceable by the pressure of the patient’s own finger, confirming retinal origin.
No theory for migraine can be complete without rationalizing its highly characteristic sex and age distribution. The futuristic template for female preponderance [Box 2, A] and age-related decline [Box 2, B] |in the prevalence of migraine is presented in the context of the eye model of human migraine, with the pathophysiologic flowchart detailed in this article maintaining hyperfocus on V1 (Figure 1) (Box 2).
| Box 2: |
| A. Factors Associated with Preponderance of Migraine in Females (human). |
|
|
|
|
|
|
|
|
| B. Factors Associated with Declining Prevalence of Migraine with Pregnancy (second and third trimesters), Menopause and Advancing Age (human). |
|
|
|
| C. Objectives of Future Advances in creation of Ideal Therapeutic Strategy for Migraine. |
| Prophylaxis, Topical or Oral, or Combined |
|
|
|
|
|
| Adapted from: Gupta VK. Adaptive Mechanisms in Migraine [16]. |
Finally, in the present article, the physiologic basis of the psychologic stress / poststress phenomenon in migraine has evolved, through the cause-effect-adaptive pathophysiologic nexus via the AVP-5HT-NA continuum as a generalized neurophysiologic mechanism relevant to neuroscience beyond primary headache. The clinical migraine-IOP-glaucoma continuum has also been elucidated with a substantial wide-based evidentiary base. Cortical spreading depression (CSD) has already been established to subserve an adaptive-protective-homeostatic role in lower mammals (rodents) and insects (Locusts and Drosophila). A pathologic role for CSD in human neurologic diseases is purely speculative. CSD/SD suppression in the neurocritical unit cannot be justified.
In summary, this N-of-1 study advances the role of sustained ocular hypotension through topical BOS 0.3% for migraine prophylaxis with a remarkable reduction in the frequency of episodic headache attacks or headache days. Persistent interictal changes in RNFL and choroid with a possible role of intraocular barotrauma are presented. Displaceable, non-homonymous, and temporal visual field-localized SS with eye-cover and digital displacement tests is reported, establishing the retina as the source of origin of positive scotomata of migraine. Pathophysiologic role of ANS hypofunction-choroidal blood flow-IOP nexus has been advanced. Key role of subclinical choroido-retinal arterial overperfusion and venous congestion, with primary or rebound increase of hydrostatic pressure generated aqueous humor and, ultimately, IOP in a wide variety of clinical circumstances and human experiments is presented. The basis of the migraine-IOP-glaucoma continuum is discussed in the context of congenital heart disease, including Ebstein anomaly, atrial septal defect, coarctation of the aorta, and patent foramen ovale, as well as in morbid obesity. An idiosyncratic and variable threshold of cumulative algogenic traffic in V1 determines the occurrence of protean migraine attacks. Arteriovenous congestion-mediated selective V1 pronociceptive traffic results in the spontaneous onset of migraine attacks for 4 hours - 72 hours. Self-tamponade mechanism of physiologic systems of eye limits ocular globe-expansion, eventually terminating corneoscleral distention and V1 algogenic traffic, with the spontaneous offset of migraine attacks. The template for female preponderance, menopause- and age-related decline in prevalence, and the fundamental requisites to evolve an ideal strategy for migraine prophylaxis has been proposed.
25 steps to certitude – eye v/s brain -- migraine unveiled
- Ashina M, Katsarava Z, Do TP, Buse DC, Pozo-Rosich P, Özge A, Krymchantowski AV, Lebedeva ER, Ravishankar K, Yu S, Sacco S, Ashina S, Younis S, Steiner TJ, Lipton RB. Migraine: epidemiology and systems of care. Lancet. 2021 Apr 17;397(10283):1485-1495. doi: 10.1016/S0140-6736(20)32160-7. Epub 2021 Mar 25. PMID: 33773613.
- Ashina M, Terwindt GM, Al-Karagholi MA, de Boer I, Lee MJ, Hay DL, Schulte LH, Hadjikhani N, Sinclair AJ, Ashina H, Schwedt TJ, Goadsby PJ. Migraine: disease characterisation, biomarkers, and precision medicine. Lancet. 2021 Apr 17;397(10283):1496-1504. doi: 10.1016/S0140-6736(20)32162-0. Epub 2021 Mar 25. PMID: 33773610.
- Ashina M, Buse DC, Ashina H, Pozo-Rosich P, Peres MFP, Lee MJ, Terwindt GM, Halker Singh R, Tassorelli C, Do TP, Mitsikostas DD, Dodick DW. Migraine: integrated approaches to clinical management and emerging treatments. Lancet. 2021 Apr 17;397(10283):1505-1518. doi: 10.1016/S0140-6736(20)32342-4. Epub 2021 Mar 25. PMID: 33773612.
- Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018 Jan;38(1):1-211. doi: 10.1177/0333102417738202. PMID: 29368949.
- Pozo-Rosich P, Lucas C, Watson DPB, Gaul C, Ramsden E, Ritter S, Martelletti P, Snellman J. Burden of Migraine in Patients With Preventive Treatment Failure Attending European Headache Specialist Centers: Real-World Evidence From the BECOME Study. Pain Ther. 2021 Dec;10(2):1691-1708. doi: 10.1007/s40122-021-00331-3. Epub 2021 Oct 13. PMID: 34643891; PMCID: PMC8586314.
- Gupta VK. Reader response: Potential for treatment benefit of small molecule CGRP receptor antagonist plus monoclonal antibody in migraine therapy. Neurology. 2020.
- Martínez-Fernández A, Rueda Vega M, Quintas S, de Toledo Heras M, Díaz de Terán J, Latorre González G, Trabajos García O, Vivancos Mora J, Gago-Veiga AB. Psychosocial repercussion of migraine: is it a stigmatized disease? Neurol Sci. 2020 Aug;41(8):2207-2213. doi: 10.1007/s10072-020-04332-6. Epub 2020 Mar 14. PMID: 32172402.
- Parikh SK, Young WB. Migraine: Stigma in Society. Curr Pain Headache Rep. 2019 Feb 9;23(1):8. doi: 10.1007/s11916-019-0743-7. PMID: 30739216.
- Vilanilam GK, Badi MK, Meschia JF. Destigmatizing Migraine. Cureus. 2018 May 30;10(5):e2711. doi: 10.7759/cureus.2711. PMID: 30065904; PMCID: PMC6066189.
- Lipton RB, Tepper SJ, Silberstein SD, Kudrow D, Ashina M, Reuter U, Dodick DW, Zhang F, Rippon GA, Cheng S, Mikol DD. Reversion from chronic migraine to episodic migraine following treatment with erenumab: Results of a post-hoc analysis of a randomized, 12-week, double-blind study and a 52-week, open-label extension. Cephalalgia. 2021 Jan;41(1):6-16. doi: 10.1177/0333102420973994. Epub 2020 Dec 3. PMID: 33269951; PMCID: PMC7786390.
- Gupta VK. Pathophysiology of migraine: an increasingly complex narrative to 2020. Fut Neurol. 2019; 14. [doi.org/10.2217/fnl-2019-0003]
- Rattanawong W, Rapoport A, Srikiatkhachorn A. Neurobiology of migraine progression. Neurobiol Pain. 2022 Jun 9;12:100094. doi: 10.1016/j.ynpai.2022.100094. PMID: 35720639; PMCID: PMC9204797.
- Rosignoli C, Ornello R, Onofri A, Caponnetto V, Grazzi L, Raggi A, Leonardi M, Sacco S. Applying a biopsychosocial model to migraine: rationale and clinical implications. J Headache Pain. 2022 Aug 11;23(1):100. doi: 10.1186/s10194-022-01471-3. Erratum in: J Headache Pain. 2022 Sep 7;23(1):116. PMID: 35953769; PMCID: PMC9367111.
- Su M, Yu S. Chronic migraine: A process of dysmodulation and sensitization. Mol Pain. 2018 Jan-Dec;14:1744806918767697. doi: 10.1177/1744806918767697. Epub 2018 Apr 12. PMID: 29642749; PMCID: PMC5900816.
- Gupta VK. CSD, BBB and MMP-9 elevations: animal experiments versus clinical phenomena in migraine. Expert Rev Neurother. 2009 Nov;9(11):1595-614. doi: 10.1586/ern.09.103. PMID: 19903020.
- Gupta VK. Adaptive Mechanisms in Migraine. A Comprehensive Synthesis in Evolution. Breaking the Migraine Code. VK Gupta. (Editor). New York: Nova Science Publications, New York. 2009; 1-122.
- Mungoven TJ, Henderson LA, Meylakh N. Chronic Migraine Pathophysiology and Treatment: A Review of Current Perspectives. Front Pain Res (Lausanne). 2021 Aug 25;2:705276. doi: 10.3389/fpain.2021.705276. PMID: 35295486; PMCID: PMC8915760.
- May A, Burstein R. Hypothalamic regulation of headache and migraine. Cephalalgia. 2019 Nov;39(13):1710-1719. doi: 10.1177/0333102419867280. Epub 2019 Aug 29. PMID: 31466456; PMCID: PMC7164212.
- Hadjikhani N, Vincent M. Neuroimaging clues of migraine aura. J Headache Pain. 2019 Apr 3;20(1):32. doi: 10.1186/s10194-019-0983-2. PMID: 30943894; PMCID: PMC6734229.
- Goadsby PJ, Holland PR, Martins-Oliveira M, Hoffmann J, Schankin C, Akerman S. Pathophysiology of Migraine: A Disorder of Sensory Processing. Physiol Rev. 2017 Apr;97(2):553-622. doi: 10.1152/physrev.00034.2015. PMID: 28179394; PMCID: PMC5539409.
- Noseda R. Cerebro-Cerebellar Networks in Migraine Symptoms and Headache. Front Pain Res (Lausanne). 2022 Jul 13;3:940923. doi: 10.3389/fpain.2022.940923. PMID: 35910262; PMCID: PMC9326053.
- Yamanaka G, Suzuki S, Morishita N, Takeshita M, Kanou K, Takamatsu T, Suzuki S, Morichi S, Watanabe Y, Ishida Y, Go S, Oana S, Kashiwagi Y, Kawashima H. Role of Neuroinflammation and Blood-Brain Barrier Permutability on Migraine. Int J Mol Sci. 2021 Aug 19;22(16):8929. doi: 10.3390/ijms22168929. PMID: 34445635; PMCID: PMC8396312.
- Ferrari MD, Goadsby PJ, Burstein R, Kurth T, Ayata C, Charles A, Ashina M, van den Maagdenberg AMJM, Dodick DW. Migraine. Nat Rev Dis Primers. 2022 Jan 13;8(1):2. doi: 10.1038/s41572-021-00328-4. PMID: 35027572.
- Diener HC, Tassorelli C, Dodick DW, Silberstein SD, Lipton RB, Ashina M, Becker WJ, Ferrari MD, Goadsby PJ, Pozo-Rosich P, Wang SJ, Mandrekar J; International Headache Society Clinical Trials Standing Committee. Guidelines of the International Headache Society for controlled trials of acute treatment of migraine attacks in adults: Fourth edition. Cephalalgia. 2019 May;39(6):687-710. doi: 10.1177/0333102419828967. Epub 2019 Feb 26. PMID: 30806518; PMCID: PMC6501455.
- Diener HC, Tassorelli C, Dodick DW, Silberstein SD, Lipton RB, Ashina M, Becker WJ, Ferrari MD, Goadsby PJ, Pozo-Rosich P, Wang SJ, Houle TT, Hoek TCVD, Martinelli D, Terwindt GM; International Headache Society Clinical Trials Committee. Guidelines of the International Headache Society for controlled trials of preventive treatment of migraine attacks in episodic migraine in adults. Cephalalgia. 2020 Sep;40(10):1026-1044. doi: 10.1177/0333102420941839. Epub 2020 Jul 28. Erratum in: Cephalalgia. 2020 Aug 18;:333102420952270. PMID: 32722936.
- Mehnert J, May A. Functional and structural alterations in the migraine cerebellum. J Cereb Blood Flow Metab. 2019 Apr;39(4):730-739. doi: 10.1177/0271678X17722109. Epub 2017 Jul 24. PMID: 28737061; PMCID: PMC6446424.
- Peng KP, May A. Migraine understood as a sensory threshold disease. Pain. 2019 Jul;160(7):1494-1501. doi: 10.1097/j.pain.0000000000001531. PMID: 31219950.
- Aurora SK, Brin MF. Chronic Migraine: An Update on Physiology, Imaging, and the Mechanism of Action of Two Available Pharmacologic Therapies. Headache. 2017 Jan;57(1):109-125. doi: 10.1111/head.12999. Epub 2016 Dec 2. PMID: 27910097; PMCID: PMC6681148.
- Schulte LH, May A. Of generators, networks and migraine attacks. Curr Opin Neurol. 2017 Jun;30(3):241-245. doi: 10.1097/WCO.0000000000000441. PMID: 28240611.
- Gupta VK. Once-weekly nocturnal ocular choroidal vascular decongestion by topical long-acting timolol ophthalmic solution applied to the headache-ipsilateral eye to prevent weekend-migraine attacks: Smartphone-app assisted case report of 2 patients for 3-years and a brief mechanistic review. J Neuroscience and Neurological Surgery. 2021; 8(6) [dOI:10.31579/2578-8868/179]
- Gupta VK. Self-ocular compression maneuver immediately relieves migraine headache attacks: A case report of managing 100 attacks over 9 years and a mechanistic review. Acta Scientific Neurology. 2021; 4.8: 72-77. [https://www.actascientific.com/ASNE/pdf/ASNE-04-0407.pdf]
- Gupta VK. Reader response: Long-term safety, tolerability, and efficacy of fremanezumab in migraine: A randomized study. Neurology 2020. Submitted September 12.
- Gupta VK. Reader response: Facial presentations of migraine, TACs, and other paroxysmal facial pain syndromes. Neurology 2019. Published on September 15.
- Gupta VK. Reader response: Gray matter volume modifications in migraine: A cross-sectional and longitudinal study. Neurology. 2019 Mar 19;92(12):587. doi: 10.1212/WNL.0000000000007131. PMID: 30886078.
- Gupta VK. Cortical-spreading depression: at the razor's edge of scientific logic. J Headache Pain. 2011 Feb;12(1):45-6. doi: 10.1007/s10194-010-0287-z. Epub 2011 Jan 11. PMID: 21222137; PMCID: PMC3055985.
- Gupta V. Constipation-related migraine is linked to the effect of the Valsalva maneuver on the eye: A case report and a mechanistic review. WebmedCentral Neurology. 2010;1(12): WMC001433. [doi: 10.9754/journal.wmc.2010.001433].
- Hougaard A, Amin FM, Christensen CE, Younis S, Wolfram F, Cramer SP, Larsson HBW, Ashina M. Increased brainstem perfusion, but no blood-brain barrier disruption, during attacks of migraine with aura. Brain. 2017 Jun 1;140(6):1633-1642. doi: 10.1093/brain/awx089. PMID: 28430860.
- Gupta VK. Migrainous scintillating scotoma and headache is ocular in origin: A new hypothesis. Med Hypotheses. 2006;66(3):454-60. doi: 10.1016/j.mehy.2005.11.010. Epub 2005 Dec 13. PMID: 16356654.
- Borgdorff P. Arguments against the role of cortical spreading depression in migraine. Neurol Res. 2018 Mar;40(3):173-181. doi: 10.1080/01616412.2018.1428406. Epub 2018 Jan 19. PMID: 29350588.
- Lemale CL, Lückl J, Horst V, Reiffurth C, Major S, Hecht N, Woitzik J, Dreier JP. Migraine Aura, Transient Ischemic Attacks, Stroke, and Dying of the Brain Share the Same Key Pathophysiological Process in Neurons Driven by Gibbs-Donnan Forces, Namely Spreading Depolarization. Front Cell Neurosci. 2022 Feb 10;16:837650. doi: 10.3389/fncel.2022.837650. Erratum in: Front Cell Neurosci. 2022 Apr 26;16:917669. PMID: 35237133; PMCID: PMC8884062.
- Major S, Huo S, Lemale CL, Siebert E, Milakara D, Woitzik J, Gertz K, Dreier JP. Direct electrophysiological evidence that spreading depolarization-induced spreading depression is the pathophysiological correlate of the migraine aura and a review of the spreading depolarization continuum of acute neuronal mass injury. Geroscience. 2020 Feb;42(1):57-80. doi: 10.1007/s11357-019-00142-7. Epub 2019 Dec 9. PMID: 31820363; PMCID: PMC7031471.
- Urbach A, Baum E, Braun F, Witte OW. Cortical spreading depolarization increases adult neurogenesis, and alters behavior and hippocampus-dependent memory in mice. J Cereb Blood Flow Metab. 2017 May;37(5):1776-1790. doi: 10.1177/0271678X16643736. Epub 2016 Jan 1. PMID: 27189903; PMCID: PMC5435280.
- Spong KE, Andrew RD, Robertson RM. Mechanisms of spreading depolarization in vertebrate and insect central nervous systems. J Neurophysiol. 2016 Sep 1;116(3):1117-27. doi: 10.1152/jn.00352.2016. Epub 2016 Jun 22. PMID: 27334953; PMCID: PMC5013167.
- Rodgers CI, Armstrong GA, Robertson RM. Coma in response to environmental stress in the locust: a model for cortical spreading depression. J Insect Physiol. 2010 Aug;56(8):980-90. doi: 10.1016/j.jinsphys.2010.03.030. Epub 2010 Apr 7. PMID: 20361971.
- Rodgers CI, Armstrong GA, Shoemaker KL, LaBrie JD, Moyes CD, Robertson RM. Stress preconditioning of spreading depression in the locust CNS. PLoS One. 2007 Dec 26;2(12):e1366. doi: 10.1371/journal.pone.0001366. PMID: 18159249; PMCID: PMC2137934.
- Tamura Y, Eguchi A, Jin G, Sami MM, Kataoka Y. Cortical spreading depression shifts cell fate determination of progenitor cells in the adult cortex. J Cereb Blood Flow Metab. 2012 Oct;32(10):1879-87. doi: 10.1038/jcbfm.2012.98. Epub 2012 Jul 11. PMID: 22781335; PMCID: PMC3463886.
- Xue JH, Yanamoto H, Nakajo Y, Tohnai N, Nakano Y, Hori T, Iihara K, Miyamoto S. Induced spreading depression evokes cell division of astrocytes in the subpial zone, generating neural precursor-like cells and new immature neurons in the adult cerebral cortex. Stroke. 2009 Nov;40(11):e606-13. doi: 10.1161/STROKEAHA.109.560334. Epub 2009 Sep 24. Erratum in: Stroke. 2010 Jul;41(7):e511. PMID: 19797181.
- Yanamoto H, Miyamoto S, Tohnai N, Nagata I, Xue JH, Nakano Y, Nakajo Y, Kikuchi H. Induced spreading depression activates persistent neurogenesis in the subventricular zone, generating cells with markers for divided and early committed neurons in the caudate putamen and cortex. Stroke. 2005 Jul;36(7):1544-50. doi: 10.1161/01.STR.0000169903.09253.c7. Epub 2005 Jun 2. PMID: 15933264.
- Hao Y, Xin M, Feng L, Wang X, Wang X, Ma D, Feng J. Review Cerebral Ischemic Tolerance and Preconditioning: Methods, Mechanisms, Clinical Applications, and Challenges. Front Neurol. 2020 Sep 18;11:812. doi: 10.3389/fneur.2020.00812. PMID: 33071923; PMCID: PMC7530891.
- Drongitis D, Rainone S, Piscopo M, Viggiano E, Viggiano A, De Luca B, Fucci L, Donizetti A. Epigenetics and cortical spreading depression: changes of DNA methylation level at retrotransposon sequences. Mol Biol Rep. 2016 Aug;43(8):755-60. doi: 10.1007/s11033-016-4000-4. Epub 2016 May 12. PMID: 27169424.
- Shen PP, Hou S, Ma D, Zhao MM, Zhu MQ, Zhang JD, Feng LS, Cui L, Feng JC. Cortical spreading depression-induced preconditioning in the brain. Neural Regen Res. 2016 Nov;11(11):1857-1864. doi: 10.4103/1673-5374.194759. PMID: 28123433; PMCID: PMC5204245.
- Yanamoto H, Xue JH, Miyamoto S, Nagata I, Nakano Y, Murao K, Kikuchi H. Spreading depression induces long-lasting brain protection against infarcted lesion development via BDNF gene-dependent mechanism. Brain Res. 2004 Sep 3;1019(1-2):178-88. doi: 10.1016/j.brainres.2004.05.105. PMID: 15306252.
- Yanamoto H, Mizuta I, Nagata I, Xue J, Zhang Z, Kikuchi H. Infarct tolerance accompanied enhanced BDNF-like immunoreactivity in neuronal nuclei. Brain Res. 2000 Sep 22;877(2):331-44. doi: 10.1016/s0006-8993(00)02718-9. PMID: 10986348.
- Rangel YM, Karikó K, Harris VA, Duvall ME, Welsh FA. Dose-dependent induction of mRNAs encoding brain-derived neurotrophic factor and heat-shock protein-72 after cortical spreading depression in the rat. Brain Res Mol Brain Res. 2001 Mar 31;88(1-2):103-12. doi: 10.1016/s0169-328x(01)00037-7. PMID: 11295236.
- Kobayashi S, Harris VA, Welsh FA. Spreading depression induces tolerance of cortical neurons to ischemia in rat brain. J Cereb Blood Flow Metab. 1995 Sep;15(5):721-7. doi: 10.1038/jcbfm.1995.92. PMID: 7673367.
- Zhou N, Rungta RL, Malik A, Han H, Wu DC, MacVicar BA. Regenerative glutamate release by presynaptic NMDA receptors contributes to spreading depression. J Cereb Blood Flow Metab. 2013 Oct;33(10):1582-94. doi: 10.1038/jcbfm.2013.113. Epub 2013 Jul 3. PMID: 23820646; PMCID: PMC3790928.
- Park CG, Chu MK. Interictal plasma glutamate levels are elevated in individuals with episodic and chronic migraine. Sci Rep. 2022 Apr 28;12(1):6921. doi: 10.1038/s41598-022-10883-9. PMID: 35484312; PMCID: PMC9050726.
- Perez-Rando M, Carceller H, Castillo-Gomez E, Bueno-Fernandez C, García-Mompó C, Gilabert-Juan J, Guirado R, Pesarico AP, Nacher J. Impact of stress on inhibitory neuronal circuits, our tribute to Bruce McEwen. Neurobiol Stress. 2022 May 13;19:100460. doi: 10.1016/j.ynstr.2022.100460. PMID: 35734023; PMCID: PMC9207718.
- Pietrancosta N, Djibo M, Daumas S, El Mestikawy S, Erickson JD. Molecular, Structural, Functional, and Pharmacological Sites for Vesicular Glutamate Transporter Regulation. Mol Neurobiol. 2020 Jul;57(7):3118-3142. doi: 10.1007/s12035-020-01912-7. Epub 2020 May 30. PMID: 32474835; PMCID: PMC7261050.
- Nedergaard M, Hansen AJ. Spreading depression is not associated with neuronal injury in the normal brain. Brain Res. 1988 May 24;449(1-2):395-8. doi: 10.1016/0006-8993(88)91062-1. PMID: 3395856.
- Carlson AP, Shuttleworth CW, Mead B, Burlbaw B, Krasberg M, Yonas H. Cortical spreading depression occurs during elective neurosurgical procedures. J Neurosurg. 2017 Jan;126(1):266-273. doi: 10.3171/2015.11.JNS151871. Epub 2016 Mar 11. PMID: 26967779.
- Koroleva VI, Bures J. Rats do not experience cortical or hippocampal spreading depression as aversive. Neurosci Lett. 1993 Jan 12;149(2):153-6. doi: 10.1016/0304-3940(93)90759-e. PMID: 8474690.
- Peréz-Saad H, Bures J. Cortical spreading depression blocks naloxone-induced escape behaviour in morphine pretreated mice. Pharmacol Biochem Behav. 1983 Jan;18(1):145-7. doi: 10.1016/0091-3057(83)90265-4. PMID: 6828533.
- Huston JP, Bures J. Effects of cortical spreading depression on behaviors elicited by hypothalamic stimulation in rats. Physiol Behav. 1973 Apr;10(4):775-80. doi: 10.1016/0031-9384(73)90162-5. PMID: 4575411.
- Huston JP, Bures J. Drinking and eating elicited by cortical spreading depression. Science. 1970 Aug 14;169(3946):702-4. doi: 10.1126/science.169.3946.702. PMID: 5464304.
- Carew TJ, Crow TJ, Petrinovich LF. Lack of coincidence between neural and behavioral manifestations of cortical spreading depression. Science. 1970 Sep 25;169(3952):1339-42. doi: 10.1126/science.169.3952.1339. PMID: 5454148.
- Tamim I, Chung DY, de Morais AL, Loonen ICM, Qin T, Misra A, Schlunk F, Endres M, Schiff SJ, Ayata C. Spreading depression as an innate antiseizure mechanism. Nat Commun 2021;12(1):2206. [PMID: 33850125] [doi: 10.1038/s41467-021-22464-x]
- Melo-Carrillo A, Schain AJ, Stratton J, Strassman AM, Burstein R. Fremanezumab and its isotype slow propagation rate and shorten cortical recovery period but do not prevent occurrence of cortical spreading depression in rats with compromised blood-brain barrier. Pain. 2020 May;161(5):1037-1043. doi: 10.1097/j.pain.0000000000001791. PMID: 31895266; PMCID: PMC7166155.
- Schain AJ, Melo-Carrillo A, Stratton J, Strassman AM, Burstein R. CSD-Induced Arterial Dilatation and Plasma Protein Extravasation Are Unaffected by Fremanezumab: Implications for CGRP's Role in Migraine with Aura. J Neurosci. 2019 Jul 24;39(30):6001-6011. doi: 10.1523/JNEUROSCI.0232-19.2019. Epub 2019 May 24. PMID: 31127003; PMCID: PMC6650995.
- Huang JY, Su CC, Wang TH, Tsai IJ. Migraine and increased risk of developing open angle glaucoma: a population-based cohort study. BMC Ophthalmol. 2019 Feb 13;19(1):50. doi: 10.1186/s12886-019-1062-9. PMID: 30760249; PMCID: PMC6375150.
- Xu C, Li J, Li Z, Mao X. Migraine as a risk factor for primary open angle glaucoma: A systematic review and meta-analysis. Medicine (Baltimore). 2018 Jul;97(28):e11377. doi: 10.1097/MD.0000000000011377. PMID: 29995778; PMCID: PMC6076184.
- Pradalier A, Hamard P, Sellem E, Bringer L. Migraine and glaucoma: an epidemiologic survey of French ophthalmologists. Cephalalgia. 1998 Mar;18(2):74-6. doi: 10.1046/j.1468-2982.1998.1802074.x. PMID: 9533601.
- Phelps CD, Corbett JJ. Migraine and low-tension glaucoma. A case-control study. Invest Ophthalmol Vis Sci. 1985 Aug;26(8):1105-8. PMID: 4019101.
- Wooliscroft J, Akram R, Zuberi H, Tong B, Gu J, Hurd A, Kooner K. Predictors of Early Onset Glaucoma. Clin Ophthalmol. 2022 Jun 10;16:1925-1932. doi: 10.2147/OPTH.S360719. PMID: 35711969; PMCID: PMC9196659.
- Chen HY, Lin CL, Kao CH. Does Migraine Increase the Risk of Glaucoma?: A Population-Based Cohort Study. Medicine (Baltimore). 2016 May;95(19):e3670. doi: 10.1097/MD.0000000000003670. PMID: 27175700; PMCID: PMC4902542.
- McKendrick AM, Nguyen BN. The eye in migraine: a review of retinal imaging findings in migraine. Clin Exp Optom. 2022 Mar;105(2):186-193. doi: 10.1080/08164622.2021.1971045. Epub 2021 Sep 19. PMID: 34538219.
- Hupp SL, Kline LB, Corbett JJ. Visual disturbances of migraine. Surv Ophthalmol. 1989 Jan-Feb;33(4):221-36. doi: 10.1016/0039-6257(82)90149-7. PMID: 2652358.
- Nguyen BN, Lek JJ, Vingrys AJ, McKendrick AM. Clinical impact of migraine for the management of glaucoma patients. Prog Retin Eye Res. 2016 Mar;51:107-24. doi: 10.1016/j.preteyeres.2015.07.006. Epub 2015 Jul 29. PMID: 26232725.
- Lisicki M, Ruiz-Romagnoli E, Piedrabuena R, Giobellina R, Schoenen J, Magis D. Migraine triggers and habituation of visual evoked potentials. Cephalalgia. 2018 Apr;38(5):988-992. doi: 10.1177/0333102417720217. Epub 2017 Jul 10. PMID: 28691517.
- Magis D, Lisicki M, Coppola G. Highlights in migraine electrophysiology: are controversies just reflecting disease heterogeneity? Curr Opin Neurol. 2016 Jun;29(3):320-30. doi: 10.1097/WCO.0000000000000335. PMID: 27120104.
- Gupta VK. Migraine, cortical excitability and evoked potentials: a clinico-pharmacological perspective. Brain. 2005 Sep;128(Pt 9):E36; author reply E37. doi: 10.1093/brain/awh606. PMID: 16129875.
- Omland PM, Nilsen KB, Uglem M, Gravdahl G, Linde M, Hagen K, Sand T. Visual evoked potentials in interictal migraine: no confirmation of abnormal habituation. Headache. 2013 Jul-Aug;53(7):1071-86. doi: 10.1111/head.12006. Epub 2013 Jan 8. PMID: 23298223.
- Gupta VK. Visual function impairment in migraine: cerebral versus retinal deficit. Cephalalgia. 1993 Dec;13(6):431-3. doi: 10.1046/j.1468-2982.1993.1306431.x. PMID: 8313461.
- Gupta VK. A hypothesis for the migraine headache syndrome. Spirit of Enterprise. The 1990 Rolex Awards. Buri International, Bern, Switzerland, 1990; 155.
- Huo YJ, Thomas R, Li L, Cao K, Wang HZ, Wang NL. Comparison of Peripapillary Retinal Nerve Fiber Layer Thickness, Functional Subzones, and Macular Ganglion Cell-Inner Plexiform Layer in Differentiating Patients With Mild, Moderate, and Severe Open-angle Glaucoma. J Glaucoma. 2020 Sep;29(9):761-766. doi: 10.1097/IJG.0000000000001598. PMID: 32657819.
- Edlinger FSM, Schrems-Hoesl LM, Mardin CY, Laemmer R, Kruse FE, Schrems WA. Structural changes of macular inner retinal layers in early normal-tension and high-tension glaucoma by spectral-domain optical coherence tomography. Graefes Arch Clin Exp Ophthalmol. 2018 Jul;256(7):1245-1256. doi: 10.1007/s00417-018-3944-6. Epub 2018 Mar 9. PMID: 29523993.
- Lin X, Yi Z, Zhang X, Liu Q, Zhang H, Cai R, Chen C, Zhang H, Zhao P, Pan P. Retinal nerve fiber layer changes in migraine: a systematic review and meta-analysis. Neurol Sci. 2021 Mar;42(3):871-881. doi: 10.1007/s10072-020-04992-4. Epub 2021 Jan 13. PMID: 33439389.
- Hamurcu MS, Gultekin BP, Koca S, Ece SD. Evaluation of migraine patients with optical coherence tomography angiography. Int Ophthalmol. 2021 Dec;41(12):3929-3933. doi: 10.1007/s10792-021-01962-3. Epub 2021 Jul 22. PMID: 34291402.
- Altunisik E, Oren B. Retinal Neurovascular Structural Changes in Optical Coherence Tomography and the Relationship between These Changes and White Matter Hyperintensities in Patients with Migraine. Eur Neurol. 2021;84(6):460-471. doi: 10.1159/000518380. Epub 2021 Aug 30. PMID: 34515117.
- Gouravani M, Salehi MA, Mohammadi S, Arevalo JF. Choroidal thickness in eyes of migraine patients measured using spectral domain-optical coherence tomography: A meta-analysis. Surv Ophthalmol. 2023 Jan-Feb;68(1):67-77. doi: 10.1016/j.survophthal.2022.01.007. Epub 2022 Jan 31. PMID: 35093402.
- Karaca EE, Koçer EB, Özdek Ş, Akçam HT, Ercan MB. Choroidal thickness measurements in migraine patients during attack-free period. Neurol Sci. 2016 Jan;37(1):81-88. doi: 10.1007/s10072-015-2364-1. Epub 2015 Aug 15. PMID: 26276221.
- Colak HN, Kantarcı FA, Tatar MG, Eryilmaz M, Uslu H, Goker H, Yildirim A, Gurler B. Retinal nerve fiber layer, ganglion cell complex, and choroidal thicknesses in migraine. Arq Bras Oftalmol. 2016 Apr;79(2):78-81. doi: 10.5935/0004-2749.20160024. PMID: 27224067.
- Dervisogullari MS, Totan Y, Gençler OS. Choroid thickness and ocular pulse amplitude in migraine during attack. Eye (Lond). 2015 Mar;29(3):371-5. doi: 10.1038/eye.2014.299. Epub 2014 Dec 12. Erratum in: Eye (Lond). 2015 Mar;29(3):452. PMID: 25502868; PMCID: PMC4366466.
- Ekinci M, Ceylan E, Cağatay HH, Keleş S, Hüseyinoğlu N, Tanyildiz B, Cakici O, Kartal B. Retinal nerve fibre layer, ganglion cell layer and choroid thinning in migraine with aura. BMC Ophthalmol. 2014 May 31;14:75. doi: 10.1186/1471-2415-14-75. PMID: 24885597; PMCID: PMC4229806.
- Yener AÜ, Korucu O. Visual Field Losses in Patients with Migraine without Aura and Tension-Type Headache. Neuroophthalmology. 2017 Jan 11;41(2):59-67. doi: 10.1080/01658107.2016.1251466. PMID: 28348627; PMCID: PMC5354103.
- McKendrick AM, Badcock DR. Decreased visual field sensitivity measured 1 day, then 1 week, after migraine. Invest Ophthalmol Vis Sci. 2004 Apr;45(4):1061-70. doi: 10.1167/iovs.03-0936. PMID: 15037569.
- Lewis RA, Vijayan N, Watson C, Keltner J, Johnson CA. Visual field loss in migraine. Ophthalmology. 1989; 96:321-326. [PMID: 2710523] [doi: 10.1016/s0161-6420(89)33069-7]
- Battista J, Badcock DR, McKendrick AM. Migraine increases centre-surround suppression for drifting visual stimuli. PLoS One. 2011 Apr 11;6(4):e18211. doi: 10.1371/journal.pone.0018211. PMID: 21494594; PMCID: PMC3073931.
- Gupta VK. Reader response: Long-term efficacy and safety of erenumab: Results from 64 weeks of the LIBERTY study. Neurology 2021. Submitted on May 05, 2021.
- Gupta VK. Reader response: Effect of fremanezumab on quality of life and productivity in patients with chronic migraine. Neurology 2020. Submitted August 10.
- Noseda R, Schain AJ, Melo-Carrillo A, Tien J, Stratton J, Mai F, Strassman AM, Burstein R. Fluorescently-labeled fremanezumab is distributed to sensory and autonomic ganglia and the dura but not to the brain of rats with uncompromised blood brain barrier. Cephalalgia. 2020 Mar;40(3):229-240. doi: 10.1177/0333102419896760. Epub 2019 Dec 19. PMID: 31856583; PMCID: PMC7233263.
- Johnson KW, Morin SM, Wroblewski VJ, Johnson MP. Peripheral and central nervous system distribution of the CGRP neutralizing antibody [125I] galcanezumab in male rats. Cephalalgia. 2019 Sep;39(10):1241-1248. doi: 10.1177/0333102419844711. Epub 2019 Apr 19. PMID: 31003588.
- Basedau H, Sturm LM, Mehnert J, Peng KP, Schellong M, May A. Migraine monoclonal antibodies against CGRP change brain activity depending on ligand or receptor target - an fMRI study. Elife. 2022 May 23;11:e77146. doi: 10.7554/eLife.77146. PMID: 35604755; PMCID: PMC9126581.
- Gupta VK. Pharmacotherapeutics of migraine and the blood-brain barrier: serendipity, empiricism, hope, and hype. MedGenMed. 2006 Jun 28;8(2):89. PMID: 16926828; PMCID: PMC1785228.
- Gupta VK. Systemic hypertension, headache, and ocular hemodynamics: a new hypothesis. MedGenMed. 2006 Sep 12;8(3):63. PMID: 17406187; PMCID: PMC1781314.
- Kurian A, Reghunadhan I, Thilak P, Soman I, Nair U. Short-term Efficacy and Safety of Topical β-Blockers (Timolol Maleate Ophthalmic Solution, 0.5%) in Acute Migraine: A Randomized Crossover Trial. JAMA Ophthalmol. 2020 Nov 1;138(11):1160-1166. doi: 10.1001/jamaophthalmol.2020.3676. PMID: 33001159; PMCID: PMC7530820.
- Aggarwal D, Heim AJ, Bittel B, Ford D, Dubinsky R, Gronseth G, Hairston V, Landazuri P, Sachen F, Herbelin L, Barohn RJ. A Randomized, Double-Blinded, Placebo-Controlled, Cross Over Study Evaluating the Efficacy and Safety of Timolol Ophthalmic Solution as an Acute Treatment of Migraine. Kans J Med. 2020 Feb 26;13(Suppl 2):2-5. PMID: 32256967; PMCID: PMC7106987.
- Gratton S, Cossack M. Answering the Call: A Prospective Look at the Role of Timolol Eye Drops in the Treatment of Acute Migraine Attacks. Mo Med. 2018 Nov-Dec;115(6):520-521. PMID: 30643343; PMCID: PMC6312165.
- Cossack M, Nabrinsky E, Turner H, Abraham A, Gratton S. Timolol Eyedrops in the Treatment of Acute Migraine Attacks: A Randomized Crossover Study. JAMA Neurol. 2018 Aug 1;75(8):1024-1025. doi: 10.1001/jamaneurol.2018.0970. Erratum in: JAMA Neurol. 2018 Aug 1;75(8):1028. Erratum in: JAMA Neurol. 2018 Oct 1;75(10):1287. PMID: 29799915; PMCID: PMC6142935.
- Migliazzo CV, Hagan JC 3rd. Beta blocker eye drops for treatment of acute migraine. Mo Med. 2014 Jul-Aug;111(4):283-8. PMID: 25211851; PMCID: PMC6179466.
- Banerjee M, Findley L. Propranolol in the treatment of acute migraine attacks. Cephalalgia. 1991 Sep;11(4):193-6. doi: 10.1046/j.1468-2982.1991.1104193.x. PMID: 1742775.
- Fuller GN, Guiloff RJ. Propranolol in acute migraine: a controlled study. Cephalalgia. 1990 Oct;10(5):229-33. doi: 10.1046/j.1468-2982.1990.1005229.x. PMID: 2272092.
- Featherstone HJ. Low-dose propranolol therapy for aborting migraine. West J Med. 1983 Mar;138(3):416-7. PMID: 6858129; PMCID: PMC1021497.
- Tokola R, Hokkanen E. Propranolol for acute migraine. Br Med J. 1978 Oct 14;2(6144):1089. doi: 10.1136/bmj.2.6144.1089-a. PMID: 709242; PMCID: PMC1608141.
- Marteau TM, Bekker H. The development of a six-item short-form of the state scale of the Spielberger State-Trait Anxiety Inventory (STAI). Br J Clin Psychol. 1992 Sep;31(3):301-6. doi: 10.1111/j.2044-8260.1992.tb00997.x. Erratum in: Br J Clin Psychol. 2020 Jun;59(2):276. PMID: 1393159.
- Kiel JW. The Ocular Circulation. San Rafael (CA): Morgan & Claypool Life Sciences; 2010. PMID: 21452447.
- Gupta VK. Botulinum toxin type A therapy for chronic tension-type headache: fact versus fiction. Pain. 2005 Jul;116(1-2):166-7; author reply 167. doi: 10.1016/j.pain.2005.03.033. PMID: 15927392.
- Gupta VK. Closure of atrial septal defect and migraine. Headache. 2004 Mar;44(3):291-2. doi: 10.1111/j.1526-4610.2004.t01-2-04063.x. PMID: 15012673.
- Zhu Y, Li S, Li J, Falcone N, Cui Q, Shah S, Hartel MC, Yu N, Young P, de Barros NR, Wu Z, Haghniaz R, Ermis M, Wang C, Kang H, Lee J, Karamikamkar S, Ahadian S, Jucaud V, Dokmeci MR, Kim HJ, Khademhosseini A. Lab-on-a-Contact Lens: Recent Advances and Future Opportunities in Diagnostics and Therapeutics. Adv Mater. 2022 Jun;34(24):e2108389. doi: 10.1002/adma.202108389. Epub 2022 Apr 11. PMID: 35130584; PMCID: PMC9233032.
- Zhao Y, Hu G, Yan Y, Wang Z, Liu X, Shi H. Biomechanical analysis of ocular diseases and its in vitro study methods. Biomed Eng Online. 2022 Jul 23;21(1):49. doi: 10.1186/s12938-022-01019-1. PMID: 35870978; PMCID: PMC9308301.
- Safa BN, Wong CA, Ha J, Ethier CR. Glaucoma and biomechanics. Curr Opin Ophthalmol. 2022 Mar 1;33(2):80-90. doi: 10.1097/ICU.0000000000000829. PMID: 34954731; PMCID: PMC8828701.
- Dennyson Savariraj A, Salih A, Alam F, Elsherif M, AlQattan B, Khan AA, Yetisen AK, Butt H. Ophthalmic Sensors and Drug Delivery. ACS Sens. 2021 Jun 25;6(6):2046-2076. doi: 10.1021/acssensors.1c00370. Epub 2021 May 27. PMID: 34043907; PMCID: PMC8294612.
- Gupta VK. Orbitofrontal cortex hypometabolism, medication overuse headache, substance abuse and migraine: key pathophysiological issues. Brain. 2006 Jul;129(Pt 7):E52; author reply E53. doi: 10.1093/brain/awl119. PMID: 16803837.
- Silva GC, Góes CP, Vincent MB. Aura-like features and photophobia in sightless migraine patients. Arq Neuropsiquiatr. 2014 Dec;72(12):949-53. doi: 10.1590/0004-282X20140200. PMID: 25517643.
- Rasmussen ML. The eye amputated - consequences of eye amputation with emphasis on clinical aspects, phantom eye syndrome and quality of life. Acta Ophthalmol. 2010 Dec;88 Thesis 2:1-26. doi: 10.1111/j.1755-3768.2010.02039.x. PMID: 21108770.
- Noseda R, Kainz V, Jakubowski M, Gooley JJ, Saper CB, Digre K, Burstein R. A neural mechanism for exacerbation of headache by light. Nat Neurosci. 2010 Feb;13(2):239-45. doi: 10.1038/nn.2475. Epub 2010 Jan 10. PMID: 20062053; PMCID: PMC2818758.
- Sörös P, Vo O, Husstedt IW, Evers S, Gerding H. Phantom eye syndrome: Its prevalence, phenomenology, and putative mechanisms. Neurology. 2003 May 13;60(9):1542-3. doi: 10.1212/01.wnl.0000059547.68899.f5. PMID: 12743251.
- Custer PL, Reistad CE. Enucleation of blind, painful eyes. Ophthalmic Plast Reconstr Surg. 2000 Sep;16(5):326-9. doi: 10.1097/00002341-200009000-00004. PMID: 11021380.
- Nicolodi M, Frezzotti R, Diadori A, Nuti A, Sicuteri F. Phantom eye: features and prevalence. The predisposing role of headache. Cephalalgia. 1997 Jun;17(4):501-4. doi: 10.1046/j.1468-2982.1997.1704501.x. PMID: 9209770.
- Peatfield RC, Rose FC. Migrainous visual symptoms in a woman without eyes. Arch Neurol. 1981 Jul;38(7):466. doi: 10.1001/archneur.1981.00510070100024. PMID: 7247775.
- Koban Y, Ozlece HK, Bilgin G, Koc M, Cagatay HH, Durgunlu EI, Burcu A. Intraocular pressure and ocular biometric parameters changes in migraine. BMC Ophthalmol. 2016 May 31;16:70. doi: 10.1186/s12886-016-0258-5. PMID: 27245325; PMCID: PMC4886420.
- Gupta VK. A clinical review of the adaptive role of vasopressin in migraine. Cephalalgia. 1997 Aug;17(5):561-9. doi: 10.1046/j.1468-2982.1997.1705561.x. PMID: 9251870.
- Dodick DW. A Phase-by-Phase Review of Migraine Pathophysiology. Headache. 2018 May;58 Suppl 1:4-16. doi: 10.1111/head.13300. PMID: 29697154.
- Knapp L, Szita B, Kocsis K, Vécsei L, Toldi J. Nitroglycerin enhances the propagation of cortical spreading depression: comparative studies with sumatriptan and novel kynurenic acid analogues. Drug Des Devel Ther. 2016 Dec 20;11:27-34. doi: 10.2147/DDDT.S117166. PMID: 28053504; PMCID: PMC5191838.
- Butt JH, S Eddelien H, Kruuse C. The headache and aura-inducing effects of sildenafil in patients with migraine with aura. Cephalalgia. 2022 Sep;42(10):984-992. doi: 10.1177/03331024221088998. Epub 2022 Mar 25. PMID: 35332812.
- Khan S, Deen M, Hougaard A, Amin FM, Ashina M. Reproducibility of migraine-like attacks induced by phosphodiesterase-3-inhibitor cilostazol. Cephalalgia. 2018 Apr;38(5):892-903. doi: 10.1177/0333102417719753. Epub 2017 Jul 5. PMID: 28677994.
- Kruuse C, Thomsen LL, Birk S, Olesen J. Migraine can be induced by sildenafil without changes in middle cerebral artery diameter. Brain. 2003 Jan;126(Pt 1):241-7. doi: 10.1093/brain/awg009. PMID: 12477710.
- Kruuse C, Thomsen LL, Jacobsen TB, Olesen J. The phosphodiesterase 5 inhibitor sildenafil has no effect on cerebral blood flow or blood velocity, but nevertheless induces headache in healthy subjects. J Cereb Blood Flow Metab. 2002 Sep;22(9):1124-31. doi: 10.1097/00004647-200209000-00010. PMID: 12218418.
- Wang M, Urenjak J, Fedele E, Obrenovitch TP. Effects of phosphodiesterase inhibition on cortical spreading depression and associated changes in extracellular cyclic GMP. Biochem Pharmacol. 2004 Apr 15;67(8):1619-27. doi: 10.1016/j.bcp.2003.12.029. PMID: 15041479.
- Gerometta R, Alvarez LJ, Candia OA. Effect of sildenafil citrate on intraocular pressure and blood pressure in human volunteers. Exp Eye Res. 2011 Jul;93(1):103-7. doi: 10.1016/j.exer.2011.05.010. Epub 2011 May 30. PMID: 21651908; PMCID: PMC3138881.
- Khan S, Amin FM, Christensen CE, Ghanizada H, Younis S, Olinger ACR, de Koning PJH, Larsson HBW, Ashina M. Meningeal contribution to migraine pain: a magnetic resonance angiography study. Brain. 2019 Jan 1;142(1):93-102. doi: 10.1093/brain/awy300. PMID: 30590467.
- VanDenBrink AM, Duncker DJ, Saxena PR. Migraine headache is not associated with cerebral or meningeal vasodilatation--a 3T magnetic resonance angiography study. Brain. 2009 Jun;132(Pt 6):e112; author reply e113. doi: 10.1093/brain/awn259. Epub 2008 Oct 14. PMID: 18854326.
- Schoonman GG, van der Grond J, Kortmann C, van der Geest RJ, Terwindt GM, Ferrari MD. Migraine headache is not associated with cerebral or meningeal vasodilatation--a 3T magnetic resonance angiography study. Brain. 2008 Aug;131(Pt 8):2192-200. doi: 10.1093/brain/awn094. Epub 2008 May 23. PMID: 18502781.
- North K, Slayden A, Mysiewicz S, Bukiya A, Dopico A. Celastrol Dilates and Counteracts Ethanol-Induced Constriction of Cerebral Arteries. J Pharmacol Exp Ther. 2020 Nov;375(2):247-257. doi: 10.1124/jpet.120.000152. Epub 2020 Aug 29. PMID: 32862144; PMCID: PMC7589950.
- Bukiya A, Dopico AM, Leffler CW, Fedinec A. Dietary cholesterol protects against alcohol-induced cerebral artery constriction. Alcohol Clin Exp Res. 2014 May;38(5):1216-26. doi: 10.1111/acer.12373. Epub 2014 Mar 3. PMID: 24588122; PMCID: PMC4010119.
- de Jong PTVM, Thee EF, Straver B. Ebstein anomaly associated with retinal venular dilatation, migraine, and visual snow syndrome: a case report. BMC Ophthalmol. 2022 Feb 14;22(1):75. doi: 10.1186/s12886-022-02288-z. PMID: 35164715; PMCID: PMC8845237.
- Shi M, Luo D, Guo J, Yang D, Li Z, Zhao H. The Function of the Autonomic Nervous System in Asian Patients With Chronic Migraine. Front Neurosci. 2022 Apr 14;16:773321. doi: 10.3389/fnins.2022.773321. PMID: 35495060; PMCID: PMC9047659.
- Kristoffersen ES, Børte S, Hagen K, Zwart JA, Winsvold BS. Migraine, obesity and body fat distribution - a population-based study. J Headache Pain. 2020 Aug 6;21(1):97. doi: 10.1186/s10194-020-01163-w. PMID: 32762643; PMCID: PMC7409451.
- Reddy A, Halenda K, Cromer P, Chen L, Butler J, Raed A, Bhagatwala J, Sponseller T, Bollinger K, Zhu H, Young L, Layman D, Dong Y. The Association of Intraocular Pressure With Obesity and Cardiometabolic Risk in a Young Farmworker Population. J Glaucoma. 2021 Jan 1;30(1):24-31. doi: 10.1097/IJG.0000000000001673. PMID: 33065612.
- Rivera-Mancilla E, Al-Hassany L, Villalón CM, MaassenVanDenBrink A. Metabolic Aspects of Migraine: Association With Obesity and Diabetes Mellitus. Front Neurol. 2021 Jun 9;12:686398. doi: 10.3389/fneur.2021.686398. PMID: 34177788; PMCID: PMC8219973.
- Walter SM, Dai Z, Wang K. Obesity, Migraine, and Overlapping Comorbidities in a Rural Pediatric Population. J Neurosci Rural Pract. 2021 Jul;12(3):524-529. doi: 10.1055/s-0041-1727574. Epub 2021 May 10. PMID: 34295107; PMCID: PMC8289561.
- Cortez MM, Millsap L, Brennan KC, Campbell CL. Craniofacial Autonomic Dysfunction in Migraine: Implications for Treatment and Prognosis. J Neuroophthalmol. 2020 Mar;40(1):67-73. doi: 10.1097/WNO.0000000000000876. PMID: 31895071.
- Miglis MG. Migraine and Autonomic Dysfunction: Which Is the Horse and Which Is the Jockey? Curr Pain Headache Rep. 2018 Feb 23;22(3):19. doi: 10.1007/s11916-018-0671-y. PMID: 29476276.
- Gazerani P, Cairns BE. Dysautonomia in the pathogenesis of migraine. Expert Rev Neurother. 2018 Feb;18(2):153-165. doi: 10.1080/14737175.2018.1414601. Epub 2017 Dec 13. PMID: 29212396.
- Volman M, Mojadidi MK, Gevorgyan R, Kaing A, Agrawal H, Tobis J. Incidence of patent foramen ovale and migraine headache in adults with congenital heart disease with no known cardiac shunts. Catheter Cardiovasc Interv. 2013 Mar;81(4):643-7. doi: 10.1002/ccd.24635. Epub 2012 Nov 14. PMID: 22927216.
- Pileggi C, Papadopoli R, De Sarro C, Nobile CGA, Pavia M. Obesity, Blood Pressure, and Intraocular Pressure: A Cross-Sectional Study in Italian Children. Obes Facts. 2021;14(2):169-177. doi: 10.1159/000514096. Epub 2021 Apr 1. PMID: 33794545; PMCID: PMC8138192.
- Ahn MW, Lee JW, Shin JH, Lee JS. Relationship between intraocular pressure and parameters of obesity in ocular hypertension. Int J Ophthalmol. 2020 May 18;13(5):794-800. doi: 10.18240/ijo.2020.05.15. PMID: 32420228; PMCID: PMC7201358.
- Vo M, Ainalem A, Qiu C, Peterlin BL, Aurora SK, Williams MA. Body mass index and adult weight gain among reproductive age women with migraine. Headache. 2011 Apr;51(4):559-69. doi: 10.1111/j.1526-4610.2010.01833.x. Epub 2011 Jan 26. PMID: 21269300; PMCID: PMC3187699.
- Gidding SS, Nehgme R, Heise C, Muscar C, Linton A, Hassink S. Severe obesity associated with cardiovascular deconditioning, high prevalence of cardiovascular risk factors, diabetes mellitus/hyperinsulinemia, and respiratory compromise. J Pediatr. 2004 Jun;144(6):766-9. doi: 10.1016/j.jpeds.2004.03.043. PMID: 15192624.
- Giardini A, Moore P, Brook M, Stratton V, Tacy T. Effect of transcatheter atrial septal defect closure in children on left ventricular diastolic function. Am J Cardiol. 2005 May 15;95(10):1255-7. doi: 10.1016/j.amjcard.2005.01.062. PMID: 15878007.
- Gupta VK. Patent foramen ovale closure and migraine: science and sensibility. Expert Rev Neurother. 2010 Sep;10(9):1409-22. doi: 10.1586/ern.10.125. PMID: 20819012.
- Gupta VK. Closure of PFO: science, quasi-science, or empiricism. Cardiology. 2009;113(2):108-10. doi: 10.1159/000174289. Epub 2008 Nov 21. PMID: 19023202.
- Zhang Y, Wang H, Liu L. Patent Foramen Ovale Closure for Treating Migraine: A Meta-Analysis. J Interv Cardiol. 2022 Feb 2;2022:6456272. doi: 10.1155/2022/6456272. PMID: 35185398; PMCID: PMC8828350.
- Mojadidi MK, Kumar P, Mahmoud AN, Elgendy IY, Shapiro H, West B, Charles AC, Mattle HP, Sorensen S, Meier B, Silberstein SD, Tobis JM. Pooled Analysis of PFO Occluder Device Trials in Patients With PFO and Migraine. J Am Coll Cardiol. 2021 Feb 16;77(6):667-676. doi: 10.1016/j.jacc.2020.11.068. PMID: 33573735.
- Elbadawi A, Barssoum K, Abuzaid AS, Rezq A, Biniwale N, Alotaki E, Mohamed AH, Vuyyala S, Ogunbayo GO, Saad M. Meta-analysis of randomized trials on percutaneous patent foramen ovale closure for prevention of migraine. Acta Cardiol. 2019 Apr;74(2):124-129. doi: 10.1080/00015385.2018.1475027. Epub 2018 Jun 18. PMID: 29914296.
- Tobis JM, Charles A, Silberstein SD, Sorensen S, Maini B, Horwitz PA, Gurley JC. Percutaneous Closure of Patent Foramen Ovale in Patients With Migraine: The PREMIUM Trial. J Am Coll Cardiol. 2017 Dec 5;70(22):2766-2774. doi: 10.1016/j.jacc.2017.09.1105. PMID: 29191325.
- Mattle HP, Evers S, Hildick-Smith D, Becker WJ, Baumgartner H, Chataway J, Gawel M, Göbel H, Heinze A, Horlick E, Malik I, Ray S, Zermansky A, Findling O, Windecker S, Meier B. Percutaneous closure of patent foramen ovale in migraine with aura, a randomized controlled trial. Eur Heart J. 2016 Jul 7;37(26):2029-36. doi: 10.1093/eurheartj/ehw027. Epub 2016 Feb 22. PMID: 26908949.
- Gupta VK. Botulinum toxin--a treatment for migraine? A systematic review. Pain Med. 2006 Sep-Oct;7(5):386-94. doi: 10.1111/j.1526-4637.2006.00216.x. PMID: 17014596.
- Gupta VK. ASD closure for migraine: is there a scientific basis? Eur Heart J. 2005 Jul;26(14):1446; author reply 1446-7. doi: 10.1093/eurheartj/ehi315. Epub 2005 May 4. PMID: 15872039.
- Herd CP, Tomlinson CL, Rick C, Scotton WJ, Edwards J, Ives NJ, Clarke CE, Sinclair AJ. Cochrane systematic review and meta-analysis of botulinum toxin for the prevention of migraine. BMJ Open. 2019 Jul 16;9(7):e027953. doi: 10.1136/bmjopen-2018-027953. PMID: 31315864; PMCID: PMC6661560.
- Herd CP, Tomlinson CL, Rick C, Scotton WJ, Edwards J, Ives N, Clarke CE, Sinclair A. Botulinum toxins for the prevention of migraine in adults. Cochrane Database Syst Rev. 2018 Jun 25;6(6):CD011616. doi: 10.1002/14651858.CD011616.pub2. PMID: 29939406; PMCID: PMC6513576.
- Castrillo Sanz A, Morollón Sánchez-Mateos N, Simonet Hernández C, Fernández Rodríguez B, Cerdán Santacruz D, Mendoza Rodríguez A, Rodríguez Sanz MF, Tabernero García C, Guerrero Becerra P, Ferrero Ros M, Duate García-Luis J. Experience with botulinum toxin in chronic migraine. Neurologia (Engl Ed). 2018 Oct;33(8):499-504. English, Spanish. doi: 10.1016/j.nrl.2016.09.004. Epub 2016 Oct 21. PMID: 27776965.
- Gupta VK. Nitric oxide and migraine: another systemic influence postulated to explain a lateralizing disorder. Eur J Neurol. 1996; 3:172-174.
- V M Fde L, W H. Relevance of excitable media theory and retinal spreading depression experiments in preclinical pharmacological research. Curr Neuropharmacol. 2014 Sep;12(5):413-33. doi: 10.2174/1570159X12666140630190800. PMID: 25426010; PMCID: PMC4243032.
- Martins-Ferreira H, Ribeiro LJ. Biphasic effects of gap junctional uncoupling agents on the propagation of retinal spreading depression. Braz J Med Biol Res. 1995 Sep;28(9):991-4. PMID: 8580888.
- Martins-Ferreira H. Spreading depression: a neurohumoral reaction. Braz J Med Biol Res. 1994 Apr;27(4):851-63. PMID: 8087091.
- Wang Y, Li Y, Wang M. Involvement of CGRP receptors in retinal spreading depression. Pharmacol Rep. 2016 Oct;68(5):935-8. doi: 10.1016/j.pharep.2016.05.001. Epub 2016 Jun 27. PMID: 27362770.
- Maranhão-Filho PA, Martins-Ferreira H, Vincent MB, Ribeiro LJ, Novis SA. Sumatriptan blocks spreading depression in isolated chick retina. Cephalalgia. 1997 Dec;17(8):822-5. doi: 10.1046/j.1468-2982.1997.1708822.x. PMID: 9453269.
- de Lima VMF, Hanke W. Reversibility of excitation waves in brain and heart and the energy of interfacial water. Can reversibility be explained by it? Prog Biophys Mol Biol. 2021 Jul;162:129-140. doi: 10.1016/j.pbiomolbio.2020.11.002. Epub 2020 Dec 3. PMID: 33279573.
- Evers S, Brockmann N, Summ O, Husstedt IW, Frese A. Primary headache and migraine in headache specialists - does personal history of doctors matter? Cephalalgia. 2020 Jan;40(1):96-106. doi: 10.1177/0333102419873671. Epub 2019 Sep 3. PMID: 31480900.
- Evans RW, Lipton RB, Silberstein SD. The prevalence of migraine in neurologists. Neurology. 2003 Nov 11;61(9):1271-2. doi: 10.1212/01.wnl.0000090628.46508.d4. PMID: 14610136.
- Noseda R, Burstein R. Migraine pathophysiology: anatomy of the trigeminovascular pathway and associated neurological symptoms, cortical spreading depression, sensitization, and modulation of pain. Pain. 2013 Dec;154 Suppl 1:S44-53. doi: 10.1016/j.pain.2013.07.021. Epub 2013 Jul 25. PMID: 23891892.
- Gupta VK. Brainstem activity in migraine: primary or secondary? Arch Neurol. 2006 Sep;63(9):1347. doi: 10.1001/archneur.63.9.1347-a. PMID: 16966528.
- Roque Bravo R, Faria AC, Brito-da-Costa AM, Carmo H, Mladěnka P, Dias da Silva D, Remião F, On Behalf Of The Oemonom Researchers. Cocaine: An Updated Overview on Chemistry, Detection, Biokinetics, and Pharmacotoxicological Aspects including Abuse Pattern. Toxins (Basel). 2022 Apr 13;14(4):278. doi: 10.3390/toxins14040278. PMID: 35448887; PMCID: PMC9032145.
- Farooque U, Okorie N, Kataria S, Shah SF, Bollampally VC. Cocaine-Induced Headache: A Review of Pathogenesis, Presentation, Diagnosis, and Management. Cureus. 2020 Aug 30;12(8):e10128. doi: 10.7759/cureus.10128. PMID: 33005542; PMCID: PMC7524019.
- Sutter FK, Helbig H. Familial retinal arteriolar tortuosity: a review. Surv Ophthalmol. 2003 May-Jun;48(3):245-55. doi: 10.1016/s0039-6257(03)00029-8. PMID: 12745002.
- Victor DI, Welch RB. Bilateral retinal hemorrhages and disk edema in migraine. Am J Ophthalmol. 1977 Oct;84(4):555-8. doi: 10.1016/0002-9394(77)90451-2. PMID: 910861.
- Broadway DC, Drance SM. Glaucoma and vasospasm. Br J Ophthalmol. 1998 Aug;82(8):862-70. doi: 10.1136/bjo.82.8.862. PMID: 9828767; PMCID: PMC1722701.
- Nicolela MT, Drance SM. Various glaucomatous optic nerve appearances: clinical correlations. Ophthalmology. 1996 Apr;103(4):640-9. doi: 10.1016/s0161-6420(96)30640-4. PMID: 8618765.
- Tenório LH, Santos AC, Câmara Neto JB, Amaral FJ, Passos VM, Lima AM, Brasileiro-Santos Mdo S. The influence of inspiratory muscle training on diaphragmatic mobility, pulmonary function and maximum respiratory pressures in morbidly obese individuals: a pilot study. Disabil Rehabil. 2013;35(22):1915-20. doi: 10.3109/09638288.2013.769635. Epub 2013 May 7. PMID: 23651130.
- Ramana RK, Sanagala T, Lichtenberg R. A new angle on the Angle of Louis. Congest Heart Fail. 2006 Jul-Aug;12(4):196-9. PMID: 16894277.
- Weiss KD, Kuriyan AE, Flynn HW Jr. Central retinal vein occlusion after prolonged vomiting and repeated valsalva maneuvers associated with gastroenteritis and dehydration. Ophthalmic Surg Lasers Imaging Retina. 2014 Apr 9;45 Online:e23-5. doi: 10.3928/23258160-20140331-03. PMID: 24702759.
- Tembl J, Lago A, Sevilla T, Solis P, Vilchez J. Migraine, patent foramen ovale and migraine triggers. J Headache Pain. 2007 Feb;8(1):7-12. doi: 10.1007/s10194-007-0359-x. Epub 2007 Feb 19. PMID: 17361381; PMCID: PMC3476121.
- Sevik MO, Çam F, Aykut A, Dericioğlu V, Şahin Ö. Choroidal vascularity index changes during the Valsalva manoeuvre in healthy volunteers. Ophthalmic Physiol Opt. 2022 Mar;42(2):367-375. doi: 10.1111/opo.12935. Epub 2021 Dec 16. PMID: 34913506.
- Vaghefi E, Shon C, Reading S, Sutherland T, Borges V, Phillips G, Niederer RL, Danesh-Meyer H. Intraocular pressure fluctuation during resistance exercise. BMJ Open Ophthalmol. 2021 May 13;6(1):e000723. doi: 10.1136/bmjophth-2021-000723. PMID: 34046525; PMCID: PMC8126276.
- Vieira GM, Oliveira HB, de Andrade DT, Bottaro M, Ritch R. Intraocular pressure variation during weight lifting. Arch Ophthalmol. 2006 Sep;124(9):1251-4. doi: 10.1001/archopht.124.9.1251. PMID: 16966619.
- Gupta VK. Reader response: Association of a cyclical migraine phenotype with phenotype with disease progression: A one-year time series analysis. Submitted 13 August 2022.
- Gupta VK. Ocular compression maneuver aborts benign cough-induced headache. Headache. 2005 May;45(5):612-4. doi: 10.1111/j.1526-4610.2005.05117_4.x. PMID: 15953285.
- Gupta VK. Is benign cough headache caused by intraocular haemodynamic aberration? Med Hypotheses. 2004;62(1):45-8. doi: 10.1016/s0306-9877(03)00298-6. PMID: 14729003.
- Coleman DJ, Trokel S. Direct-recorded intraocular pressure variations in a human subject. Arch Ophthalmol. 1969 Nov;82(5):637-40. doi: 10.1001/archopht.1969.00990020633011. PMID: 5357713.
- Ioannidis JP. Why most published research findings are false. PLoS Med. 2005 Aug;2(8):e124. doi: 10.1371/journal.pmed.0020124. Epub 2005 Aug 30. Erratum in: PLoS Med. 2022 Aug 25;19(8):e1004085. PMID: 16060722; PMCID: PMC1182327.
- Feinstein AR. "Clinical Judgment" revisited: the distraction of quantitative models. Ann Intern Med. 1994 May 1;120(9):799-805. doi: 10.7326/0003-4819-120-9-199405010-00012. PMID: 8147553.
- Hokenson RE, Short AK, Chen Y, Pham AL, Adams ET, Bolton JL, Swarup V, Gall CM, Baram TZ. Unexpected Role of Physiological Estrogen in Acute Stress-Induced Memory Deficits. J Neurosci. 2021 Jan 27;41(4):648-662. doi: 10.1523/JNEUROSCI.2146-20.2020. Epub 2020 Dec 1. PMID: 33262247; PMCID: PMC7842761.
- Schoech L, Allie K, Salvador P, Martinez M, Rivas E. Sex Differences in Thermal Comfort, Perception, Feeling, Stress and Focus During Exercise Hyperthermia. Percept Mot Skills. 2021 Jun;128(3):969-987. doi: 10.1177/00315125211002096. Epub 2021 Mar 17. PMID: 33730933.
- Celik F, Edipoglu IS. Evaluation of preoperative anxiety and fear of anesthesia using APAIS score. Eur J Med Res. 2018 Sep 11;23(1):41. doi: 10.1186/s40001-018-0339-4. PMID: 30205837; PMCID: PMC6131845.
- Byrd-Bredbenner C, Eck K, Quick V. GAD-7, GAD-2, and GAD-mini: Psychometric properties and norms of university students in the United States. Gen Hosp Psychiatry. 2021 Mar-Apr;69:61-66. doi: 10.1016/j.genhosppsych.2021.01.002. Epub 2021 Jan 9. PMID: 33571925.
- Zloto O, Skaat A, Fabian ID, Rosner M, Ziv H, Leshno A, Melamed S. The distribution of relaxin receptors in the anterior segment of primary open-angle glaucoma patients. Indian J Ophthalmol. 2020 Oct;68(10):2117-2120. doi: 10.4103/ijo.IJO_2008_19. PMID: 32971620; PMCID: PMC7728022.
- Celikbilek A, Sabah S, Tanik N, Ak H, Atalay T, Yilmaz N. Is serum S100B protein an useful biomarker in migraine? Neurol Sci. 2014 Aug;35(8):1197-201. doi: 10.1007/s10072-014-1679-7. Epub 2014 Feb 16. PMID: 24531979.
- Hampel U, Klonisch T, Sel S, Schulze U, Garreis F, Seitmann H, Zouboulis CC, Paulsen FP. Insulin-like factor 3 promotes wound healing at the ocular surface. Endocrinology. 2013 Jun;154(6):2034-45. doi: 10.1210/en.2012-2201. Epub 2013 Mar 28. Erratum in: Endocrinology. 2014 Jan;155(1):331. Garreis, Fabian [added]; Seitmann, Holger [added]; Zouboulis, Christos C [added]. PMID: 23539510.
- Goldsmith LT, Weiss G. Relaxin in human pregnancy. Ann N Y Acad Sci. 2009 Apr;1160:130-5. doi: 10.1111/j.1749-6632.2008.03800.x. PMID: 19416173; PMCID: PMC3856209.
- Tzourio C, El Amrani M, Robert L, Alpérovitch A. Serum elastase activity is elevated in migraine. Ann Neurol. 2000 May;47(5):648-51. PMID: 10805337.
- Pieretti S, Di Giannuario A, Di Giovannandrea R, Marzoli F, Piccaro G, Minosi P, Aloisi AM. Gender differences in pain and its relief. Ann Ist Super Sanita. 2016 Apr-Jun;52(2):184-9. doi: 10.4415/ANN_16_02_09. PMID: 27364392.
- Hu R, McDonough AA, Layton AT. Sex differences in solute and water handling in the human kidney: Modeling and functional implications. iScience. 2021 May 29;24(6):102667. doi: 10.1016/j.isci.2021.102667. PMID: 34169242; PMCID: PMC8209279.
- Taradaj K, Ginda T, Maciejewicz P, Suchonska B, Wielgos M, Kecik D, Kociszewska-Najman B. Does pregnancy influence eye parameters? Assessment of choroidal thickness using EDI-OCT before and after labour depending on the way of delivery method. Ginekol Pol. 2020;91(11):668-673. doi: 10.5603/GP.a2020.0137. PMID: 33301160.
- Roskal-Wałek J, Laudańska-Olszewska I, Biskup M, Gierada M, Odrobina D. Choroidal Thickness in Women with Uncomplicated Pregnancy: Literature Review. Biomed Res Int. 2017;2017:5694235. doi: 10.1155/2017/5694235. Epub 2017 Nov 9. PMID: 29250544; PMCID: PMC5700513.
- Jastaniah N, Sagim RA, Sanyour RM, Alamri DM, Bajandouh RH, Shaheen EA, Althubaiti A. A Retrospective Chart Review: The Prevalence of Hyponatremia Among Elderly Inpatients in a Tertiary Care Centre in Saudi Arabia. Cureus. 2022 Mar 8;14(3):e22960. doi: 10.7759/cureus.22960. PMID: 35411259; PMCID: PMC8989247.
- Filippatos TD, Makri A, Elisaf MS, Liamis G. Hyponatremia in the elderly: challenges and solutions. Clin Interv Aging. 2017 Nov 14;12:1957-1965. doi: 10.2147/CIA.S138535. PMID: 29180859; PMCID: PMC5694198.
- Dastiridou AI, Ginis HS, De Brouwere D, Tsilimbaris MK, Pallikaris IG. Ocular rigidity, ocular pulse amplitude, and pulsatile ocular blood flow: the effect of intraocular pressure. Invest Ophthalmol Vis Sci. 2009 Dec;50(12):5718-22. doi: 10.1167/iovs.09-3760. Epub 2009 Jul 15. PMID: 19608534.
- Pallikaris IG, Kymionis GD, Ginis HS, Kounis GA, Tsilimbaris MK. Ocular rigidity in living human eyes. Invest Ophthalmol Vis Sci. 2005 Feb;46(2):409-14. doi: 10.1167/iovs.04-0162. PMID: 15671262.
- Afridi S, Kaube H, Goadsby PJ. Occipital activation in glyceryl trinitrate induced migraine with visual aura. J Neurol Neurosurg Psychiatry. 2005 Aug;76(8):1158-60. doi: 10.1136/jnnp.2004.050633. PMID: 16024898; PMCID: PMC1739768.
- Ailani J. A Practical Approach to Autonomic Dysfunction in Patients with Headache. Curr Neurol Neurosci Rep. 2016 May;16(5):41. doi: 10.1007/s11910-016-0641-x. PMID: 27021770.
- Alkozi HA, Navarro G, Franco R, Pintor J. Melatonin and the control of intraocular pressure. Prog Retin Eye Res. 2020 Mar;75:100798. doi: 10.1016/j.preteyeres.2019.100798. Epub 2019 Sep 25. PMID: 31560946.
- Alkozi H, Sánchez-Naves J, de Lara MJ, Carracedo G, Fonseca B, Martinez-Aguila A, Pintor J. Elevated intraocular pressure increases melatonin levels in the aqueous humour. Acta Ophthalmol. 2017 May;95(3):e185-e189. doi: 10.1111/aos.13253. Epub 2016 Sep 6. PMID: 27595784.
- Barrachina-Esteve O, Hidalgo-Torrico I, Acero C, Aranceta S, Cánovas-Vergé D, Ribera G. Visual snow syndrome and its relationship with migraine. Neurologia 2021;S0213-4853(21)00112-2. [PMID: 34521544] [doi: 10.1016/j.nrl.2021.05.012]
- Birk S, Kruuse C, Petersen KA, Jonassen O, Tfelt-Hansen P, Olesen J. The phosphodiesterase 3 inhibitor cilostazol dilates large cerebral arteries in humans without affecting regional cerebral blood flow. J Cereb Blood Flow Metab. 2004 Dec;24(12):1352-8. doi: 10.1097/01.WCB.0000143536.22131.D7. PMID: 15625409.
- Butt JH, Rostrup E, Hansen AS, Lambertsen KL, Kruuse C. Induction of migraine-like headache, but not aura, by cilostazol in patients with migraine with aura. Brain. 2018 Oct 1;141(10):2943-2951. doi: 10.1093/brain/awy228. PMID: 30137217.
- Celikbilek A. Migraine symptoms and the role of autonomic dysfunction. Eur J Neurol. 2020 Dec;27(12):e97. doi: 10.1111/ene.14504. Epub 2020 Sep 21. PMID: 32888332.
- Christensen CE, Younis S, Lindberg U, de Koning P, Tolnai D, Paulson OB, Larsson HBW, Amin FM, Ashina M. Intradural artery dilation during experimentally induced migraine attacks. Pain. 2021 Jan;162(1):176-183. doi: 10.1097/j.pain.0000000000002008. PMID: 32701652.
- Cursiefen C, Wisse M, Cursiefen S, Jünemann A, Martus P, Korth M. Migraine and tension headache in high-pressure and normal-pressure glaucoma. Am J Ophthalmol. 2000 Jan;129(1):102-4. doi: 10.1016/s0002-9394(99)00289-5. PMID: 10653426.
- Falkenberg K, Bjerg HR, Olesen J. Subcutaneous sumatriptan reduces cilostazol induced headache in migraine patients. Cephalalgia. 2020 Jul;40(8):842-850. doi: 10.1177/0333102420915166. Epub 2020 Mar 26. PMID: 32216457.
- Fraser CL, Hepschke JL, Jenkins B, Prasad S. Migraine Aura: Pathophysiology, Mimics, and Treatment Options. Semin Neurol. 2019 Dec;39(6):739-748. doi: 10.1055/s-0039-1700525. Epub 2019 Dec 17. PMID: 31847045.
- Gupta VK. Reader Response: Blood-Brain Barrier Permeability in Patients With Reversible Cerebral Vasoconstriction Syndrome Assessed With Dynamic Contrast-Enhanced MRI. Neurology. 2022 Mar 1;98(9):382-383. doi: 10.1212/WNL.0000000000013318. PMID: 35228316.
- Gupta VK. Interatrial shunt-associated migraine: serendipity, empiricism, hope, or hype? Stroke. 2006 Sep;37(9):2212; author reply 2213. doi: 10.1161/01.STR.0000237167.80526.13. Epub 2006 Aug 10. PMID: 16902169.
- Gupta VK. Cortical spreading depression is neuroprotective: the challenge of basic sciences. Headache. 2005 Feb;45(2):177-8; author reply 178. doi: 10.1111/j.1526-4610.2005.05039_1.x. PMID: 15705129.
- Gupta VK. Migraine, epilepsy, and brain neuronal hyperexcitation. Headache. 2005 Jan;45(1):89; author reply 89-90. doi: 10.1111/j.1526-4610.2005.05019.x. PMID: 15663624.
- Gupta VK. Closure of ASD: what aggravates the migrainous diathesis? Eur Heart J. 2006 Jul;27(14):1756-7. doi: 10.1093/eurheartj/ehl070. Epub 2006 Jun 7. PMID: 16760211.
- Gupta VK. Does magnesium supplementation have any role in acute myocardial infarction? No. Cardiovasc Drugs Ther. 1996 Jul;10(3):303-5. doi: 10.1007/BF02627952. PMID: 8877071.
- Gupta VK. Patent foramen ovale/atrial septal defect closure and migraine: searching the rationale for the procedure. J Am Coll Cardiol. 2005 Aug 16;46(4):737-8; author reply 738-9. doi: 10.1016/j.jacc.2005.05.029. PMID: 16098448.
- Gupta VK. Clopidogrel and atrial shunt closure for migraine: why is migraine aggravated immediately? Heart 2005. Comment on: Wilmshurst. 2005;91(9):1173-1175.[PMID: 16103551] [doi: 10.1136/hrt.2004.047746] Available at: https://heart.bmj.com/content/91/9/1173.responses#clopidogrel-and-atrial-shunt-closure-for-migraine-why-is-migraine-aggravated-immediately
- Gupta VK. Glyceryl trinitrate and migraine: nitric oxide donor precipitating and aborting migrainous aura. J Neurol Neurosurg Psychiatry 2005.
- Harris A, Kagemann L, Ehrlich R, Ehrlich Y, López CR, Purvin VA. The effect of sildenafil on ocular blood flow. Br J Ophthalmol. 2008 Apr;92(4):469-73. doi: 10.1136/bjo.2007.131789. PMID: 18369062.
- Hickner J. New-and surprising-ways to approach migraine pain. J Fam Pract. 2022 Jun;71(5):198-218. doi: 10.12788/jfp.0432. PMID: 35776873.
- Hodak J, Fischer U, Bassetti CLA, Schankin CJ. Episodic Visual Snow Associated With Migraine Attacks. JAMA Neurol. 2020 Mar 1;77(3):392-393. doi: 10.1001/jamaneurol.2019.4050. PMID: 31764944; PMCID: PMC6902200.
- Hwang DJ, Shin JY, Yu HG. Oral Administration of Cilostazol Increases Ocular Blood Flow in Patients with Diabetic Retinopathy. Korean J Ophthalmol. 2017 Apr;31(2):123-131. doi: 10.3341/kjo.2017.31.2.123. Epub 2017 Mar 21. PMID: 28367040; PMCID: PMC5368085.
- Iser C, Arca K. Headache and Autonomic Dysfunction: a Review. Curr Neurol Neurosci Rep. 2022 Oct;22(10):625-634. doi: 10.1007/s11910-022-01225-3. Epub 2022 Aug 22. PMID: 35994191.
- Katz BJ. Put a Drop of Timolol Into Each Eye and Call Me in the Morning. JAMA Ophthalmol. 2020 Nov 1;138(11):1166-1167. doi: 10.1001/jamaophthalmol.2020.3837. PMID: 33001150.
- Khawaja AP, Chan MP, Broadway DC, Garway-Heath DF, Luben R, Yip JL, Hayat S, Wareham NJ, Khaw KT, Foster PJ. Systemic medication and intraocular pressure in a British population: the EPIC-Norfolk Eye Study. Ophthalmology. 2014 Aug;121(8):1501-7. doi: 10.1016/j.ophtha.2014.02.009. Epub 2014 Apr 2. PMID: 24702754; PMCID: PMC4109027.
- Koksal M, Ozdemir H, Kargi S, Yesilli C, Tomaç S, Mahmutyazicioglu K, Mungan A. The effects of sildenafil on ocular blood flow. Acta Ophthalmol Scand. 2005 Jun;83(3):355-9. doi: 10.1111/j.1600-0420.2005.00422.x. PMID: 15948790.
- Panicker G, Kaliaperumal S, Narayan S, Mani M. Glaucoma and optical coherence tomography changes in migraine: A comparative cross-sectional study. Indian J Ophthalmol. 2021 Dec;69(12):3546-3551. doi: 10.4103/ijo.IJO_375_21. PMID: 34826993; PMCID: PMC8837329.
- Plaisier E, Ronco P. COL4A1-Related Disorders. 2009 Jun 25 [updated 2016 Jul 7]. In: Adam MP, Feldman J, Mirzaa GM, Pagon RA, Wallace SE, Bean LJH, Gripp KW, Amemiya A, editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993–2023. PMID: 20301768.
- Rangel YM, Karikó K, Harris VA, Duvall ME, Welsh FA. Dose-dependent induction of mRNAs encoding brain-derived neurotrophic factor and heat-shock protein-72 after cortical spreading depression in the rat. Brain Res Mol Brain Res. 2001 Mar 31;88(1-2):103-12. doi: 10.1016/s0169-328x(01)00037-7. PMID: 11295236.
- Vance SK, Imamura Y, Freund KB. The effects of sildenafil citrate on choroidal thickness as determined by enhanced depth imaging optical coherence tomography. Retina. 2011 Feb;31(2):332-5. doi: 10.1097/IAE.0b013e3181eef0ae. PMID: 20975620.
- P Vilela MA, Colossi CG, Freitas HP, Valle GD, Pellanda LC. Ocular Alterations Associated with Primary Congenital Heart Disease - A Cross-sectional Study. Middle East Afr J Ophthalmol. 2020 Apr 29;27(1):28-33. doi: 10.4103/meajo.MEAJO_89_19. PMID: 32549721; PMCID: PMC7276169.
- Wang JJ, Mitchell P, Smith W. Is there an association between migraine headache and open-angle glaucoma? Findings from the Blue Mountains Eye Study. Ophthalmology. 1997 Oct;104(10):1714-9. doi: 10.1016/s0161-6420(97)30075-x. PMID: 9331214.
- Wu F, Zhao Y, Zhang H. Ocular Autonomic Nervous System: An Update from Anatomy to Physiological Functions. Vision (Basel). 2022 Jan 14;6(1):6. doi: 10.3390/vision6010006. PMID: 35076641; PMCID: PMC8788436.