More Information
Submitted: April 28, 2025 | Approved: May 06, 2025 | Published: May 07, 2025
How to cite this article: Levi RM, Csaba HDL. Bidirectional Aspects of Well-being of Patients and Main Caregivers after Neurosurgery. J Neurosci Neurol Disord. 2025; 9(1): 046-051. Available from:
https://dx.doi.org/10.29328/journal.jnnd.1001109
DOI: 10.29328/journal.jnnd.1001109
Copyright License: © 2025 Levi RM, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Well-being; Neurosurgery; Mobility; Primary caregiver
Bidirectional Aspects of Well-being of Patients and Main Caregivers after Neurosurgery
Rivka Mor Levi* and Habil Dégi L Csaba
Sheba Medical Center, Derech Sheba 2, Tel Hashomer, Ramat Gan, Israel
*Address for Correspondence: Rivka Mor Levi, Sheba Medical Center, Derech Sheba 2, Tel Hashomer, Ramat Gan, Israel, Email: [email protected]
Objectives: Hospitalization following a head injury is associated with high rates of disability that have a strong correlation with depression, anxiety, and low self-esteem. Well-being is related to life satisfaction, quality of life, happiness, personal growth and flourishing, competence, self-acceptance, positive relationships, and autonomy. The well-being of patients and their primary caregivers is important when a patient is left with impaired mobility after neurosurgery. The aim of this study is to examine whether the well-being of patients and their primary caregivers will differ before and after neurosurgery, and whether well-being differs between patients with motor disability (WMD group) and those without, compared to those who are not - NMD group (non-motor disability).
Methodology: 123 patients and their main caregivers were recruited. Of these, 62 were in the before neurosurgical group, 31 Patients and 31 caregivers. 61 in the after neurosurgical group, 30 Patients and 31 caregivers, of which there are 16 from WMD group and 15 from NMD.
Main outcome measures: Two analyses of Variance (ANOVA) were conducted: for WMD and NMD separately. The results reveal a significant decrease in wellbeing for both, patient and main caregivers, but a stronger decline in well-being was observed among WMD, as indicated by a larger effect size (η² = 0.74) compared to the NMD (η² = 0.38). In addition, no significant effect between group and time of measurement was found, indicating that the decrease in wellbeing was not different among patients compared to their main caregivers.
Conclusion: The findings highlight the multifaceted impact of neurosurgery on well-being, particularly for patients who remain with motor disabilities and their primary caregivers.
The decline in well-being after neurosurgery highlights the need for improved social support and the importance of developing treatment programs that can help ease the process of coping with these phenomena and provide appropriate support for both patients and their primary caregivers.
The official definition of neurosurgery by the American Board of Neurological Surgery ABNS is: “Medical discipline and surgical specialty that provides treatment in pain or pathological processes that may alter the function or activity of the central, peripheral and the autonomic nervous system”. Neurosurgery is among the youngest and most developing surgical disciplines [1].
Hospitalization following a head injury is associated with high rates of disability even 5-7 years later. Disability development shows a strong correlation with measures of depression, anxiety, and low self-esteem [2]. One year after a traumatic brain injury, approximately a quarter of patients reported disability requiring personal assistance. One-third of them experienced problems with social integration, and 42% were neither employed nor received a salary. Nearly half of the patients reported poor physical health, and 37% reported poor mental health [3].
In recent years, evidence has accumulated regarding the relationship between low mobility during hospitalization and long-term functional impairment, the need for transition to institutional care, recurrent hospitalizations, and increased risk of mortality [4]. Head injury is associated with short-term morbidity and mortality, and is linked to decreased long-term survival time, underscoring the importance of measures aimed at prevention and clinical interventions to reduce morbidity and mortality due to head injury [5].
Mobility is defined as the ability of a person to move from one point to another independently or with the help of aids within the house, the street, the city and the country where he lives Meyer, Janke & Beaujean, 2014. Among people over 65 years of age, mobility is one of the most important functions and has the most significant impact on their well-being Forte, Boreham, De Vito & Pesce, 1998; World Health Organization, 2002. Moreover, Traumatic Brain Injury (TBI) is considered a potential modifiable dementia risk factor among the elderly [6].
Hospitalized patients spend more than 80% of their time in bed and spend less than 43 minutes walking per day. For hospitalized patients with low physical mobility, there is a 34 times greater chance of death, and a six times greater likelihood of needing hospitalization compared to those who undergo mobility two or more times a day Smart, et al. 2018. Among patients under the age of 65, 57% of their hospitalization time is spent in bed, 33.6% is spent sitting and only 9% is spent standing or walking Mudge, et al. 2016.
Due to the significant short-term and long-term implications of mobility, particularly those with brain injuries, it is crucial to understand the meaning of impaired mobility. This understanding can help improve outcomes, impact the patient’s ability to perform daily tasks, and facilitate a successful return to functioning within society. Thereby mobility can contribute to social cohesion and strengthening the healthcare system when the individual is discharged from the hospital and reintegrates into society and the community they live in, especially considering that Posttraumatic Amnesia (PTA) is a common outcome of TBI [7].
Patients after Neurosurgery experience more disability, and it takes longer to recover in the postoperative period compared to lighter surgeries. Also, treating patients after craniectomy Part of the skull is temporarily removed to relieve intracranial pressure, usually due to traumatic brain injury, is psychologically demanding, which leads to an increase in the main caregiver’s burden [8].
Many people willingly take on the role of main caregiver. Informal caregivers who provided care, help, and support experienced greater burdens and higher levels of stress and depression. The impact on burden and psychological well-being becomes more pronounced when the informal caregiver has a close relationship or lives in the same household as the care recipient/patient [9].
Therefore, it is important to understand how it affects their Well-being. Community integration for individuals with disabilities supports the individual and the well-being of the entire community Dubé, 2023. There is a growing awareness of the importance of well-being and satisfaction with life, both among individuals and among policy makers [10].
While most contemporary research argues that well-being is multidimensional and related to how individuals, communities, and societies feel when they are successful, there is no single agreed-upon definition. Well-being is related to positive and negative effects, life satisfaction, quality of life, happiness, personal growth and flourishing, competence, self-acceptance, positive relationships, and autonomy Dodge, Daly, Huyton, & Sanders, 2012. Complications after neurosurgical operations can have a serious impact on the patient’s well-being [11].
Well-being is a term used synonymously with a wide range of concepts including self-esteem, self-efficacy, self-determination, resilience, quality of life, improved mood, positive mental health, life satisfaction, and worth Huppert, 2017.
Improved well-being has been shown to lead to better life outcomes in terms of health, satisfying social relationships, higher productivity, and educational achievement. This is relevant to policy makers working in the field, as it enables the design of new policies, comparing the costs and benefits of different interventions [10]. Complications after neurosurgical operations can have a serious impact on well-being [11].
To date, studies have been conducted on the association between reduced mobility during hospitalization and long-term functional impairment. Relatively little research has been conducted documenting the experiences and well-being of the primary caregiver, as well as the aspects that influence the well-being of patients after neurosurgery, especially those who remain with impaired mobility after neurosurgery.
A quantitative design using closed-ended questionnaires was employed in this study. The aim of the first stage in the study was to examine the patients’ and their main caregivers’ well-being before neurosurgery. The aim of the second stage in the study was to examine whether the patients’ and their main caregivers’ well-being after the neurosurgery, and accordance group: NMD (non-motor disability) or WMD (with motor disability).
Research hypothesis was that the patients’ and their main caregivers’ wellbeing will decrease significantly after the neurosurgery. However, the patients and main caregivers from the WMD group will exhibit a greater decrease in wellbeing compared to the NMD group. Regarding the question of whether the degree of decrease will significantly differ between patients and their main caregiver, no previous research was conducted and therefore no hypothesis was made regarding this difference.
The research independent variable was Time: before and after neurosurgery, and Study groups: patients (and their main caregiver) whose neurosurgery led to a motor disability (WMD group), patients (and their main caregiver) whose neurosurgery did not lead to a motor disability (NMD group).
The dependent variables were Patients’ and their main caregivers’ wellbeing.
The study participant included adult patients over the age of 18 who were hospitalized in the neurosurgical department of a large medical center in a central medical center in the Middle East during 2024–2025. The patients were hospitalized due to an acute neurosurgical problem or exacerbation of a chronic condition. Patients who were unable to answer the questionnaires due to their condition, such as patients with delirium or unconsciousness, were not invited to participate. Likewise, patients whose condition was defined as terminal were not invited to participate.
Inclusion criteria were age 18 and older, hospitalized in the neurosurgery department and eligible and capable of providing informed consent.
Instruments
In this study, the questionnaire WHO-5 Well-being Index Bech, 1998, was selected as a research tool, and a demographic questionnaire that reflects the characteristics of the participants in the study. The World Health Organization- Five Well-Being Index (WHO-5) is a short self-reported measure of current mental wellbeing.
The WHO-5 has been found to have adequate validity in screening and measuring outcomes in clinical trials. Item response theory analyses in studies of younger persons and elderly persons indicate that the measure has good construct validity as a unidimensional scale measuring well-being in these populations [12]. The selection of the research tool was made after a thorough examination of the purpose of the study, the question and the context in which the study is being conducted.
Statistics analysis
To examine whether the dependent variables are normally distributed, tests were conducted for each study group (WMD, NMD). Both non-parametric analyses and parametric analyses were conducted to examine the research questions and hypotheses. To examine the research question regarding the differences between the two time points, the two study groups and the subject in their wellbeing, three-way mixed ANOVA (2x2x2) analyses were conducted for the well-being measures.
Data collection procedures and ethical consideration
The study consisted of two phases. In the first phase, conducted between October 2024 and November 2024, the research questionnaires were distributed to pre-neurosurgery, patients and main caregivers.
In the second phase, conducted between December 2024 and January 2025, the research questionnaires were distributed to the postoperative patients and main caregivers, divided into mobile and non-mobile disabilities.
The research team included the principal investigator, and a student assigned as a research assistant. Participants were approached directly, introduced themselves and provided a comprehensive explanation of the study and its importance, ensured anonymity, and explained the duration and conditions. The questionnaires were completed in the participants’ own time on the premises of the department where they were staying.
Anonymization of personally identifiable information: the ethics of the data do not allow it to be associated with a specific person. In the case of this study, no personal identifiable information is stored so that information cannot be linked to specific users. Informed consent is obtained from each study participant. The data is not transferred to any party. The study received approval from the ethics committee of the hospital where the patients were admitted to the neurosurgical department and approval from the ethics committee of the University of Cluj.
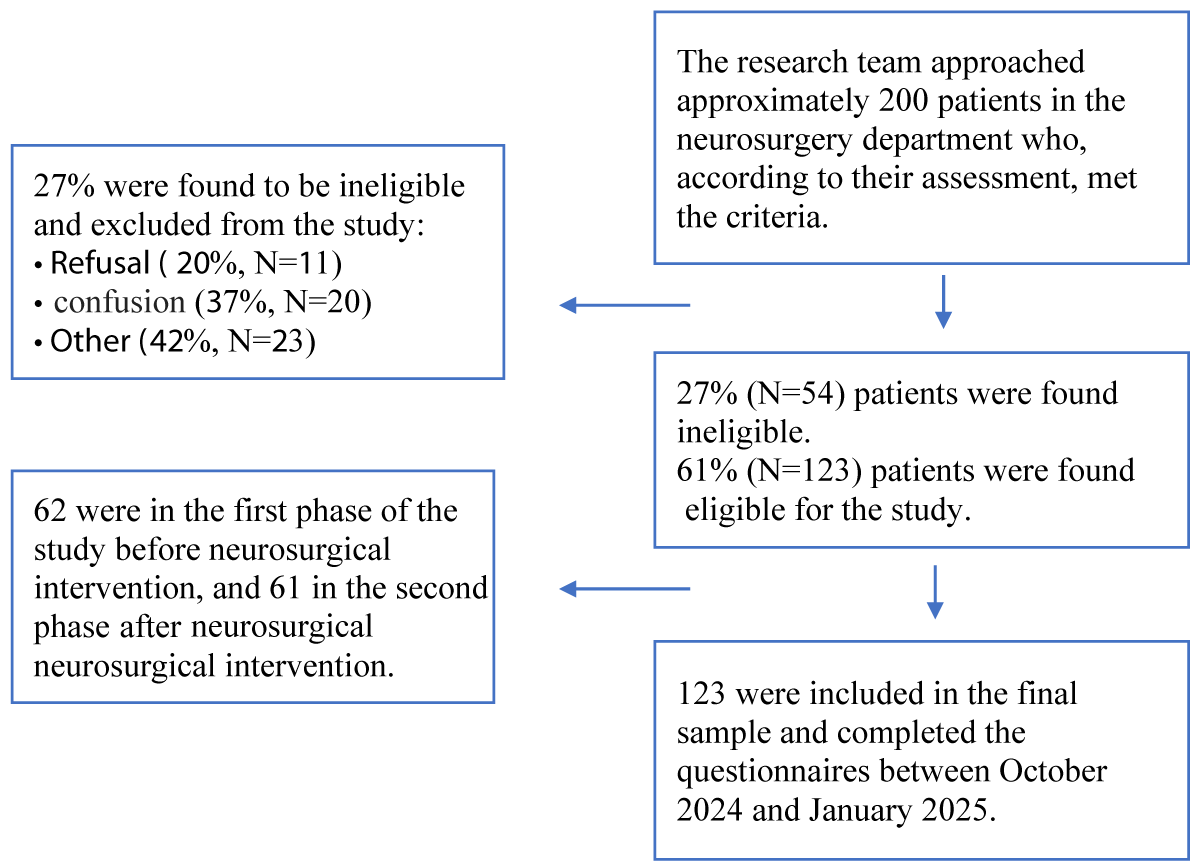
The research team approached over 200 potential patients. 27% of them were found to be ineligible to participate according to the inclusion criteria or refused to participate. The main reasons for exclusion were a state of consciousness or alertness that made it impossible to sign an informed consent.
About 6.5% of those who were defined as eligible were later diagnosed by the staff in the ward as having confusion that rendered them ineligible to participate in the study. The main reasons for refusal were fear of exposure or fear of family members that prevented the patient from participating and refusal to sign an informed consent. Some potential participants did not agree to give a reason for their refusal.
In total, 123 patients and the main caregivers were recruited for the study.
Of these, 62 were in the first phase of the study before neurosurgical intervention, of which there are 31 patients and another 31 main caregivers, and 61 in the second phase after neurosurgical intervention of which there are 30 patients and another 31 main caregivers.
Figure 1 describes the circumstances of non-enrollment and dropout in the study groups.
Figure 1: Circumstances of non-enrollment and dropout in the study groups.
The first hypothesis was: The patients’ and their main caregivers’ wellbeing will decrease significantly after the neurosurgery. However, the patients and main caregivers from the WMD group will exhibit a greater decrease in wellbeing compared to the NMD group.
To examine the hypothesis, Analysis of Variance (ANOVA) was conducted: Time of measurement (Pre / Post) X Group (patients / caregivers) with wellbeing as the dependent variable. Two analyses were conducted: for WMD and NMD separately.
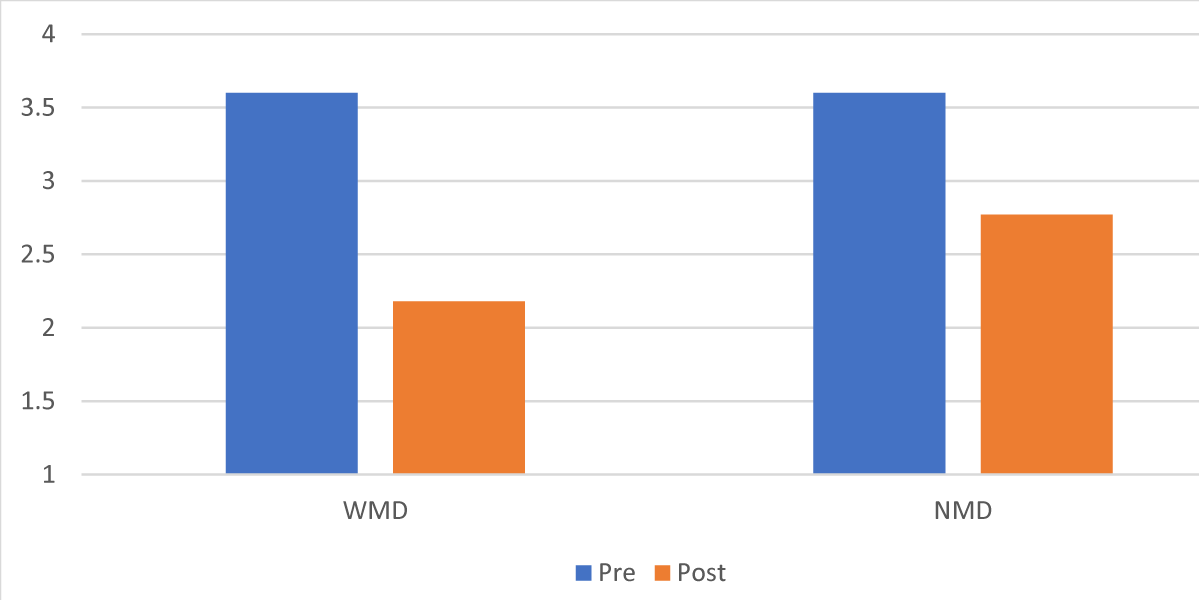
Table 1 and Figure 2 present the means and standard deviations of the level of wellbeing, by time of measurement and group. Table 2 presents the ANOVA results.
| Table 1: Means and standard deviations (SDs) of well-being by time and group (WMD, NMD). | |||||
| WMD | |||||
| Patients | Caregivers | Total | |||
| Pre (24) | Post (16) | Pre (31) | Post (15) | Pre (55) | Post (31) |
| 3.60 (0.46) | 2.12 (0.41) | 3.60 (0.35) | 2.24 (0.43) | 3.60 (0.40) | 2.18 (0.42) |
| NMD | |||||
| Patients | Caregivers | Total | |||
| Pre (24 | Post (16) | Pre (31 | Post (15) | Pre (55) | Post (31) |
| 3.60 (0.46) | 2.73 (0.75) | 3.60 (0.35) | 2.81 (0.56) | 3.60 (0.40) | 2.77 (0.65) |
| Table 2: Results of ANOVA on changes in wellbeing. | ||||
| WMD | NMD | |||
| F (1,82) | η2 | F | η2 | |
| Time | 235.51 | 0.74 | 51.66*** | 0.38 |
| Time * Group | 0.37 | 0.001 | 0.13 | 0.001 |
| *** p < .001 | ||||
Figure 2: Changes in well-being among WMD and NMD.
The results reveal a significant decrease in wellbeing , but the level of decrease is stronger among WMD- with motor disability participants, as indicated by a larger size effect (η² = 0.74) compared to the NMD (η2 = 0.38). In addition, no significant effect between group and time of measurement was found, indicating that the decrease in wellbeing was not different among patients compared to their main caregivers. The hypothesis was supported.
Neurosurgery represents a medical intervention with the potential to significantly alter patients’ and their main caregiver’s health trajectories and wellbeing. While advances in surgical techniques have improved outcomes, the broader impact of neurosurgery on patients’ and their main caregiver’s well-being remains a critical area of investigation.
This study addresses a gap in the literature by examining the differential effects of neurosurgery on two distinct patient groups—those with motor disability following neurosurgery and those without—while also considering the experiences of their main caregivers. Understanding how neurosurgery influences well-being is essential for developing more comprehensive pre- and post-operative care strategies and mostly when those patients go back into society.
The findings reveal a significant decrease in well-being following neurosurgery for both groups of patients, before and after, with a more pronounced decrease among participants with motor disability (WMD) compared to those without motor disability (NMD) after neurosurgery. This result supports previous research indicating that individuals with motor disabilities often experience heightened psychological distress, reduced wellbeing, and greater dependence on main caregivers after medical interventions [13].
A possible explanation for this finding is that the physical limitations imposed by motor impairments may contribute to increased frustration, loss of autonomy, and diminished participation in daily activities, all of which are known factors influencing the well-being WHO, 2011.
Interestingly, the absence of a significant interaction effect between group and time of measurement suggests that the decline in well-being was comparable between patients and their main caregivers. This finding is consistent with existing literature highlighting the bidirectional nature of patient-caregiver distress [14].
Main caregivers often experience emotional strain as they navigate the challenges of providing support, adjusting to changes in their loved one’s functional status, and managing their own psychological well-being. The fact that well-being declined for both groups, regardless of whether they were patients or caregivers, highlights the need for holistic interventions that address not only the medical and rehabilitative needs of patients but also the psychological and social support needs of the main caregivers [15].
These findings have significant implications for post-operative care. First, they emphasize the necessity of targeted psychological and rehabilitative interventions for patients with motor disabilities, as they are at higher risk for deteriorating well-being. Rehabilitation programs should incorporate mental health support, occupational therapy, and social integration strategies to mitigate the psychological toll of motor impairments.
Second, the results reinforce the importance of caregiver support programs, as caregivers experience well-being declines like patients. Caregiver burden is a well-documented issue in medical caregiving contexts, and interventions such as psychoeducational programs, peer support groups, and respite care may be crucial in preserving caregiver well-being and, by extension, enhancing patient outcomes [16].
The significant decrease in well-being observed in the WMD group indicates the urgent need to develop treatment and rehabilitation programs that will begin before surgery like meetings with a clinical psychologist or social worker to coordinate expectations, manage fears, and build resilience. During the last week of hospitalization, focus on training sessions for the patient and the main caregiver on the expected daily routine at home, practice of basic care techniques, proper lifting, feeding, hygiene, use of medical devices, information on rights, benefits, and continued care in the community.
After surgery, a caregiver support group, led by a trained therapist, meets (psychologist, social worker) once a week, shares mental and physical difficulties, and receives tools for good communication with the patient and for self-care, emotional support, share experiences, deal with functional changes, feelings of loneliness and loss, strengthen coping skills, and create a sense of belonging. Additionally, a digital platform for home support could include reminders for breathing exercises, log mood, submit questions, receive medication reminders, guided exercises, and video tutorials may also support continued care at home.
The study has several limitations, including sample size, and in particular the subgroups of patients with and without postoperative motor disability, which may limit generalizability to a broader population. Second, the study used only two time-point measurements without long-term follow-up to examine changes in well-being over time. Finally, potential confounding variables such as prior psychiatric history or type of neurosurgical procedure, which may have had a significant impact on the study results, were not examined.
The findings highlight the multifaceted impact of neurosurgery on well-being, particularly for individuals with motor disabilities. Addressing the social dimensions of recovery is crucial in improving long-term outcomes for both patients and their main caregivers.
The conclusion derived from the research findings is that neurosurgery, despite the medical benefits it may offer, brings with it significant challenges on both emotional and social levels for both patients and main caregivers. The observed decline in well-being after neurosurgery highlights the need for enhanced social support following neurosurgical procedures. It also underscores the importance of developing therapeutic programs that can help ease the coping process with these effects and provide appropriate support to both patients and their main caregivers. Future interventions should adopt a comprehensive, interdisciplinary approach, integrating medical, psychological, and social care strategies to enhance post-surgical well-being.
- Barrow DL, Bendok BR. Introduction: What is Neurosurgery? Oper Neurosurg (Hagerstown). 2019;17(Suppl 1):S1-S2. Available from: https://doi.org/10.1093/ons/opz071
- Whitnall L, McMillan TM, Murray GD, Teasdale GM. Disability in young people and adults after head injury: 5–7 years follow up of a prospective cohort study. J Neurol Neurosurg Psychiatry. 2006;77(5):640-5. Available from: https://doi.org/10.1136/jnnp.2005.078246
- Andelic N, Sigurdardottir S, Schanke AK, Sandvik L, Sveen U, Roe C. Disability, physical health and mental health 1 year after traumatic brain injury. Disabil Rehabil. 2010;32(13):1122-31. Available from: https://doi.org/10.3109/09638280903410722
- Duan-Porter W, Vo TN, Ullman K, Langsetmo L, Strotmeyer ES, Taylor BC, et al. Hospitalization-associated change in gait speed and risk of functional limitations for older adults. J Gerontol A Biol Sci Med Sci. 2019;74(10):1657-63. Available from: https://doi.org/10.1093/gerona/glz027
- Elser H, Gottesman RF, Walter AE, Coresh J, Diaz-Arrastia R, Mosley TH, et al. Head injury and long-term mortality risk in community-dwelling adults. JAMA Neurol. 2023;80(3):260-9. Available from: https://doi.org/10.1001/jamaneurol.2022.5024
- Raj R, Kaprio J, Pekka J, Korja M, Siironen J. Risk of dementia after hospitalization due to traumatic brain injury. Neurology. 2022;98(23):e2377-86. Available from: https://doi.org/10.1212/wnl.0000000000200290
- Ponsford J, Trevena-Peters J, Janzen S, Harnett A, Marshall S, Patsakos E, et al. INCOG 2.0 guidelines for cognitive rehabilitation following traumatic brain injury, Part I: Posttraumatic amnesia. J Head Trauma Rehabil. 2023;38(1):24-37. Available from: https://doi.org/10.1097/htr.0000000000000840
- Leong KW, Li L, Moga R, Bernstein M, Venkatraghavan L. Assessment of caregiver burden in patients undergoing in- and out-patient neurosurgery. J Clin Neurosci. 2021;88:83-7. Available from: https://doi.org/10.1016/j.jocn.2021.03.035
- Malki ST, Johansson P, Andersson G, Andréasson F, Mourad G. Caregiver burden, psychological well-being, and support needs among Swedish informal caregivers. BMC Public Health. 2025;25:867. Available from: https://doi.org/10.1186/s12889-025-22074-y
- Maccagnan A, Wren-Lewis S, Brown H, Taylor T. Wellbeing and society: towards quantification of the co-benefits of wellbeing. Soc Indic Res. 2019;141(1):217-43. Available from: https://doi.org/10.1007/s11205-017-1826-7
- Comfort LD, Neidert MC, Bozinov O, Regli L, Stienen MN. Determining the impact of postoperative complications in neurosurgery based on simulated longitudinal smartphone app-based assessment. Acta Neurochir (Wien). 2022;164(1):207-17. Available from: https://doi.org/10.1007/s00701-021-04967-0
- Winther Topp C, Ostergaard SD, Søndergaard S, Bech P. The WHO-5 Well-Being Index: A systematic review of the literature. Psychother Psychosom. 2015;84(3):167-76. Available from: https://doi.org/10.1159/000376585
- Krahn GL, Klein Walker D, Correa-De-Araujo R. Persons with disabilities as an unrecognized health disparity population. Am J Public Health. 2015;105(Suppl 2):S198-206. Available from: https://doi.org/10.2105/AJPH.2014.302182
- Pinquart M, Sörensen S. Correlates of physical health of informal caregivers: A meta-analysis. J Gerontol B Psychol Sci Soc Sci. 2007;62(2):P126-37. Available from: https://doi.org/10.1093/geronb/62.2.P126
- Adelman RD, Tmanova LL, Delgado D, Dion S, Lachs MS. Caregiver burden: A clinical review. JAMA. 2014;311(10):1052-60. Available from: https://doi.org/10.1001/jama.2014.304
- Schulz R, Sherwood PR. Physical and mental health effects of family caregiving. Am J Nurs. 2008;108(9 Suppl):23-7; quiz 27. Available from: https://doi.org/10.1097/01.naj.0000336406.45248.4c